Auditor: KY Medicaid wasted $800 million. Health secretary cites ‘significant inaccuracies.’

By Sarah Ladd
Kentucky Lantern
Kentucky Auditor Allison Ball alleges in a report released Wednesday that the state mismanaged about $800 million in taxpayer funds, resulting in payments to Medicaid managed care organizations at the same time other states were paying for the same patients.
Dr. Steven Stack, secretary of the Cabinet for Health and Family Services, called the Wednesday report a “rehash” of what federal investigators found in 2022 — that 47 states made capitation payments for Medicaid recipients who were enrolled in two states. Medicaid is a federal-state program that pays for 1 in 3 Kentuckians’ health care.

“The issue of concurrent enrollment in Medicaid Managed Care was identified by a federal inspector general in 2022 and is happening in nearly all 50 states, making the (auditor’s) ‘special examination’ a rehash,” Stack wrote in a Sept. 10 letter to Ball, which is included in the report.
Kentucky Medicaid contracts with six insurance companies to serve as managed care organizations (MCOs) that offer competing health plans and process claims. Medicaid pays the MCOs a set amount called a capitation payment for each patient.
As “one of Kentucky’s costliest programs,” Ball said in a statement, “it’s essential that we make sure every Medicaid dollar spent is going directly to benefit Kentuckians in need of services, not being wasted due to bureaucratic negligence.”
The audit says Kentucky was one of four states — along with Ohio, Oregon and Washington — that were asked by federal officials during the Biden administration to dig into state-specific issues related to concurrent payments to MCOs from Jan. 1, 2019, to Dec. 31, 2022. An auditor spokesperson said the office examined these dates because the Office of Inspector General “specifically asked us to look at this time period.”
Among other things, the report suggests, as a solution, that managed care organizations carry more responsibility in their contracts to help track members and eliminate waste.
“The issues causing this waste are straightforward problems that can be fixed with relative ease,” the report said.
Tyler Glick, spokesman for the Kentucky Association of Health Plans, which represents the state’s managed care organizations, said in a statement that the MCOs are not to blame for this problem.
MCOs “are obligated to cover medical services for enrolled Kentuckians,” Glick said in a statement. But: “health plans don’t decide who is eligible.”

“Existing federal rules cap profits and require actuarial rate-setting, limiting concurrent spending. Kentucky’s health plans improve Medicaid by coordinating high-quality, whole-person care, emphasizing preventive services and promoting competition and consumer choice,” Glick said. “As always, health plans remain committed to working with state and federal officials to ensure program efficiency and continuity of care.”
The auditor’s report, Stack said in his Sept. 10 letter, “contains significant inaccuracies, relies heavily on unsubstantiated assumptions and fails to provide verifiable evidence of any substantial loss of taxpayer funds.”
Stack also wrote that the report lacked a determination of the “actual state of residence for each overlapping month” and “a significant portion of the counted overlap happened during time periods when Kentucky Medicaid was the correct state of residence instead of the other state, and vice versa.”
In a response letter, Ball said that “whether Kentucky or another state is the true state of residency for those concurrently enrolled individuals matters only for determining whether more of that waste falls on the shoulders of Kentucky taxpayers or another state’s taxpayers” but asserted that “Kentucky taxpayers have shouldered the burden of this waste in at least some capacity as federal taxpayers.”
Stack said states also lack “access to the data necessary to identify when beneficiaries are concurrently enrolled in a Medicaid Managed Care program in another state.” Ball responded in a letter dated Sept. 17: “That is false. At a base level, CHFS already does have all the data it needs to identify concurrent enrollment.”
In July, the Centers for Medicare and Medicaid Services announced several plans to “partner with states to reduce duplicate enrollment.” Stack referenced that promise in his letter to the auditor and said, “Our agency has yet to receive any additional guidance.”
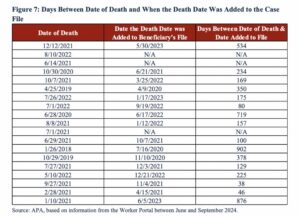
Ball’s report also alleges that there were delays in recording deaths and ceasing payments to MCOs. Looking at a sample of 19 Medicaid patients who died, the report says Kentucky made payments for at least four months after the date of death. The Cabinet for Health and Family Services took an average of 320 days to “reflect the deaths” of those Kentuckians, the report says.
In Stack’s response letter, he says that the cabinet relies on official records of deaths and “there are reasons why that could be delayed.”
Ball’s Sept. 17 letter says the auditor’s office “cannot confirm nor deny whether (the cabinet) truly removed 56,440 individuals from Medicaid during the examined period. Regardless, its failure to address the issues outlined in the (auditor’s) report contributed to over $800 million of Medicaid waste borne by United States taxpayers.”
Kendra Steele, a spokeswoman for the cabinet, said the report fails to “acknowledge states depend on federal partners to see through their commitment to provide the necessary guidance and technical assistance.”
“We know what the issue is because (the Office of Inspector General) and (Centers for Medicaid Services) have told us: States need full access to the tools necessary to identify concurrent enrollment,” she said. “(The cabinet) stands ready to take action as soon as that information is provided by the federal government.”
In her Sept. 17 letter to Stack, Ball wrote that the cabinet has a “reactive, and not proactive, vision for addressing the issue,” which she called “concerning.”
“As the Auditor of Public Accounts has outlined in its report, (the cabinet) can take numerous steps right now to address this issue without federal government guidance,” Ball wrote. “It should take those steps while the Trump administration prepares to give states tools for combating this issue that previous administrations have not.”
Read the full report here.