Government Accountability Office says Medicare and Medicaid each overpaid health-care providers by about $50 billion in 2023
Improper payments, mainly through overpayments, in Medicare and Medicaid are expected to total about $50 billion each for 2023, the federal Government Accountability Office says in its annual report on the topic. Both programs showed declines in improper payments from 2022: $11 billion in Medicare and about $30 billion in Medicaid, the latter due mainly to “the end of states’ Covid-19 flexibilities, including the suspension of eligibility determinations and provider enrollment requirements,” reports Amy Lotven of Inside Health Policy.
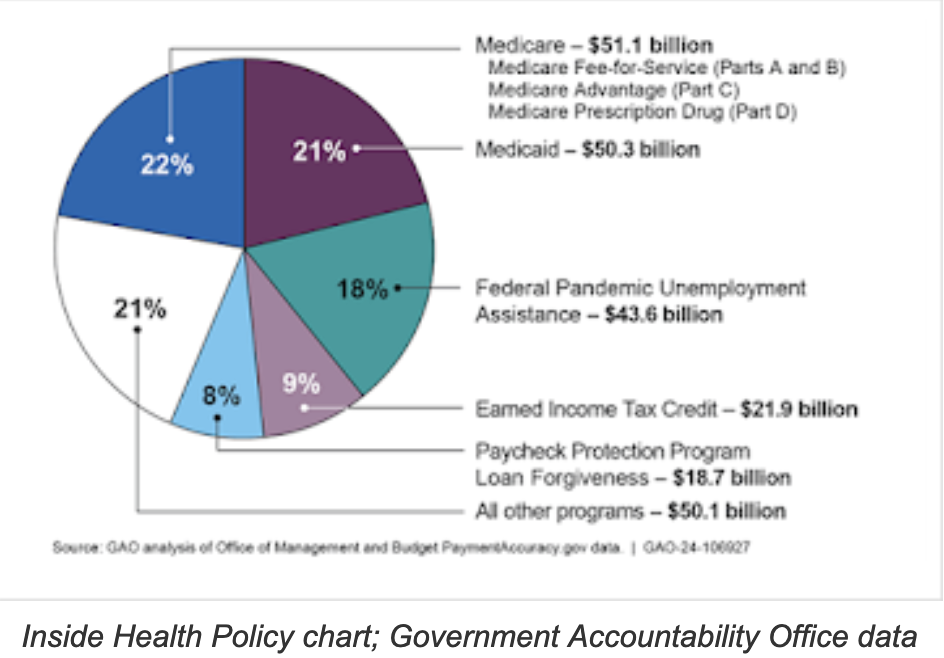
The GAO estimated total improper federal payments in 2023 would be $236 billion, but noted that the projections “do not include certain programs that have been determined susceptible to improper payments: for example, the Temporary Assistance for Needy Families programs; and the government-wide total potentially does not represent the full extent of improper payments,” Lotven reports.
About $175 billion of the improper payments are overpayments, “while $44.6 billion were labeled ‘unknown,’ meaning GAO was unable to determine whether they were proper or improper,” Lotven writes. “$11.5 billion were underpayments and $4.6 billion were technically improper because they failed to follow all applicable regulations even though the recipient was entitled to the funding.”
While improper Medicare payments declined overall, they increased in Medicare Advantage, the privately run version of the prohram, whoch now serves most Medicare beneficiaries. GAO estimated improper Advantage payments at $17 billion in 2023, up from $12.8 billion in 2022.