Child obesity is a complex problem, intimidating to those who are fighting it (last in a series)
 |
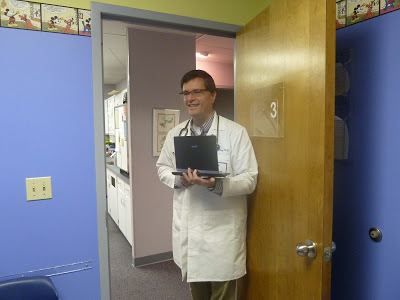
| Dr. Christopher Bolling prepares to see a patient. |
By Tara Kaprowy
Kentucky Health News
Nearly every weekday, pediatrician Christopher Bolling starts his day by scooping up his lap top and stepping into one of his cheerfully-appointed exam rooms. After greeting his young patients, who are generally passing the time by playing games on their parents’ cell phones, Bolling begins his examinations. During his 21 years of practice, those exams have increasingly ended with Bolling counseling parents about their children’s weight.
“I tell them I’m not worried about this as a cosmetic issue, I’m worried about this as a health issue,” he said in an interview. “This isn’t about your child being ugly or undesirable, we talk about them being healthy and not healthy.”
But, though dedicated to his cause, Bolling, of Crestview Hills in Kenton County, said he is keenly aware that his counseling is not nearly enough to help his patients overcome the weight that is impeding their health. “What makes this problem unique is it is so multifactorial, there are so many pieces to it,” he said. “It’s food, it’s activity, it’s portion size, it’s fruit and vegetables, it’s screen time and safety. And it makes it really intimidating to know what to do with it.”
“We’re swimming upstream in a flooded river,” agreed Debra Cotterill, director of the Nutrition Education Program at the University of Kentucky. “Even for people who know it, it’s still hard. Weight is an issue I have to address every single day of my life and I understand how it is for people. You’re talking about change of behaviors.”
It’s like smoking, but it’s different
But a sweeping change in behavior is going to be what it takes to turn the tide of the obesity epidemic, experts say, and that is one reason fighting obesity is often likened to the battle against smoking. The fact that it is just as, if not more, deadly is another parallel, as is the fact that it is just as, if not more, far-reaching.
But there are key differences in battling the two problems, Judith Graham noted in a story for Kaiser Health News. First, other than an increase in health-care costs, there is no compelling argument that implies that another person’s weight adversely affects others, like second-hand smoking does for smoking, or drunk driving does for drinking to excess. “The notion that my behavior as a smoker can have an effect on you and can make you sick was critically important in accelerating people’s intolerance of smoking and their willingness to see the government take action,” Michael Ericksen, director of the Institute of Public Health at Georgia State University, told Graham.
Compounding the issue is there is nearly no end to the variety of food that can contribute to the problem. Unlike Big Tobacco, the food industry also cannot be demonized as easily, Graham points out. But most importantly, “unlike alcohol and tobacco, you can’t go cold turkey on food,” Bolling said. “You have to keep eating.”
But if there is consensus on how to approach the issue, it is to take a lesson from the battle against smoking, which is to focus on changing the environment that encourages bad habits. “It’s about changing our culture,” explained Elaine Russell, Kentucky’s obesity prevention coordinator. “We need an environment where the healthy choice is the easy choice.”
That involves policy change, setting up systems that support the policy changes, and environmental change, Russell said, all of which have to happen together. “There’s no one solution that’s going to do it,” she said. “If we embed it in our policies, but we don’t embed it into our environment, how do we make the healthier choice? If we just educate people but we don’t provide them with a healthy environment, then how do they make those healthy choices? We could do an educational campaign at our worksite, but if we have unhealthy vending machines there, how can you make the changes?”
Local action is needed
Russell said change needs to happen at the local level, since every community has different needs and “starts with high-level partners really being engaged,” she said. “We need to pull together those leaders and ask them what the highest priority is, ask them what feasibly can be done and start checking them off.”
Some of those changes can be as easy as placing bananas and apples at the front of the pool concession stand so children see them first, as they did in Lexington. The same is being done in school cafeteria lines. But others cost money that communities don’t necessarily have, as the Healthy Children’s Task Force learned in Laurel County when trying to assess students’ body-mass index, a rough measure of fat to weight.
In 2005, the task force started collecting BMIs of a select group of children in kindergarten to see where the county stood. It found 37 percent were either overweight or obese, and quickly decided the goal should be to bring that number down to 31 percent, the statewide average at the time. Using a grant from the parent company of the local hospital, they talked to parents, hired gym teachers, had schools incorporate 10 minutes of physical activity in the classroom periodically during the day, talked to kids about nutrition, and got them to cook and sample fruit and vegetables from a mobile demonstration kitchen.
The overweight rates of the children, who were repeatedly assessed each year, did decrease by the targeted 6 percent, but when funding ran out, the program faltered. For a few years, part of the effort was restored, but the task force has disbanded. “You get real gung-ho on it and something else comes along,” said school nurse Duff Holcomb, who led the effort. “It makes me feel terribly guilty, but that is just the way it is. We proved what works.”
After a recent analysis showed 12 states, including Kentucky, have adult obesity levels over 30 percent, Jeffrey Levi, executive director of Trust for America’s Health, acknowledged the financial problem: “We’re not investing anywhere near what we need to in order to bend the obesity curve and see the returns in health and savings.”
 |
| (Photos by Tara Kaprowy) |
More regulation is one option, a move that is generally cheap in cost but can be politically expensive. New York City Mayor Michael Bloomberg is learning that, after proposing a ban in New York City on the sale of supersize sodas and other sugary drinks by restaurants, movie theaters and street carts. Residents are deeply divided on the issue — 60 percent oppose the ban — and critics have lambasted Bloomberg, accusing him of running a “nanny state.”
But limiting food and drink choices may have an effect on people’s health, a recent study indicates. The removal of trans fats from many processed and fast foods like French fries and cookies probably reduced the proportion of kids with high cholesterol in the past decade, researchers think.
More regulation, particularly in how food is marketed to children, is what Josh Golin, associate director for the Campaign for Commercial-Free Childhood, would like to see. “We can’t rely on the companies to self-regulate or develop their own policies,” he said. “We see a lot of self-serving regulations that vary from company to company. What we really need is to level the playing field and make the rules enforceable.”
In addition, Bolling suggested “there are several organizations that advocate that we could make a big impact on childhood obesity by placing an excise tax on sodas.” A report by the Rudd Center for Food Policy and Obesity at Yale University indicated that a 10 percent tax on soft drinks would result in about an 8 percent reduction in consumption. Studies on alcohol and tobacco taxes indicate similar findings. A Rudd Center calculator shows a 1-cent tax on each ounce of sugar-sweetened beverages sold in Kentucky could result in nearly $200 million in revenue for the state.
Whether regulation or investing more money in the problem are part of the solution, Bolling said solving the problem will take time and a variety of efforts. “We have to solve everything together,” he said. “It’s about personal responsibility, but it’s also about supportive families, it’s about primary care medical people knowing what to say to their patients, it’s about workplaces and schools creating good environments and it’s communities providing opportunities to be healthy. I think we’re going to turn the tide. We’ve done it before with seat belts, with bicycle helmets, with smoking. While this problem is complicated, we already see people really waking up to it.”
Kentucky Health News is a service of the Institute for Rural Journalism and Community Issues, based in the School of Journalism and Telecommunications at the University of Kentucky, with support from the Foundation for a Healthy Kentucky.