Essential-benefits rule expands mental-health and substance-abuse coverage; Ky. needs more facilities to treat newly eligible
The
Department of Health and Human Services has defined the 10 “essential health benefits” insurance plans must provide, and it included benefits for mental health and treatment of substance-abuse disorders..
Nearly 20 percent of Americans don’t have access to mental-health services and over 30 percent have no coverage for substance-abuse treatment. This rule will expand mental health and substance-abuse treatment benefits to 62 million Americans, according to HHS.
Expanded coverage for mental health and substance abuse treatment programs in Kentucky could bring about a dramatic shift in the delivery of these services. There is already a shortage of treatment options and centers for Kentuckians, and those suffering from addiction have not had coverage for such treatment; the proposed rule will change that.
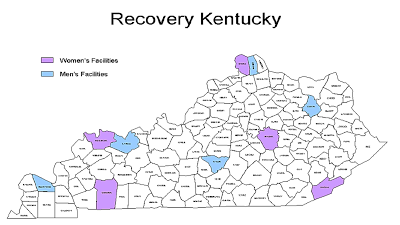
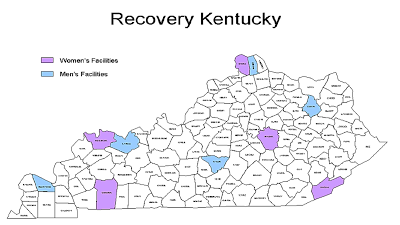
Recovery Kentucky, a public-private partnership with residential facilities, was created to help Kentuckians recover from substance abuse. It has 10 centers, in Campbellsville, Erlanger, Florence, Harlan, Henderson, Hopkinsville, Morehead, Owensboro, Paducah, and Richmond,
according to the 2012
Justice & Public Safety Cabinet report, which included the map below.
Health-insurance plans must cover the 10 essential benefits beginning in 2014, so the state must prepare for the newly insured in addition to newly covered services. The rule defines what must be covered in insurance plans and bans discrimination based on age or pre-existing conditions. Among the core package of items and services, known as “essential health benefits” are items and services in the following categories:
- Ambulatory patient services
- Emergency services
- Hospitalization
- Maternity and newborn care
- Mental health and substance use disorder services, including behavioral health treatment
- Prescription drugs
- Rehabilitative and habilitative services and devices
- Laboratory services
- Preventive and wellness services and chronic disease management
- Pediatric services, including oral and vision care
States are given flexibility in implementing the federal health-care reform law with a benchmark approach. The Kentucky Department of Insurance has recommended that the Anthem Preferred Provider Organization plan serve as the “benchmark” plan for the Kentucky Health Benefit Exchange. HHS will review the recommendation and accept public comments prior to making a final decision. (Read more)