As health care expands and more providers are needed, pressure grows to allow nurse practitioners more prescribing authority
Kentucky Health News
As Kentucky expands Medicaid and implements the Affordable Care Act, more Kentuckians will have health coverage and access to care, worsening Kentucky’s already existing shortage of physicians, particularly those providing primary care in rural areas. And, as the stakes get higher, so do tensions between physicians and nurse practitioners about how newly covered Kentuckians will receive their care.
Nurse practitioners say part of the solution involves removing their requirement to have a “collaborative agreement” with a doctor to write prescriptions. Nurse practitioners have been pushing for years to get rid of this requirement, saying they have the expertise to independently prescribe non-scheduled or routine drugs like cholesterol medications, reports Laura Ungar of The Courier-Journal in an article about the NPs’ debate with physicians.
Doctors say collaborative agreements are necessary to protect patients, and call for a team-based approach to health care, writes Ungar. “My hope is the collaborative agreement will be strengthened,” Dr. Shawn Jones of Paducah, past president of the Kentucky Medical Association, told Ungar. “Certainly, physician manpower is an issue in Kentucky and in the U.S. … but there’s not a great amount of evidence that collaborative agreements impair nurse practitioners from performing their duties.” But Ungar’s story notes that NPs sometimes have trouble finding a collaborating physician.
Legislation to let NPs prescribe non-scheduled drugs without a doctor agreement passed the state House but failed in the Senate this year. The NPs aren’t giving up, and many are working with state Sen. Paul Hornback, R-Shelbyville, on a similar bill for the next legislative session. Most agree that collaborative agreements are appropriate in the case of controlled substances, such as narcotic painkillers, but other wish to prescribe other drugs too, reports Ungar.
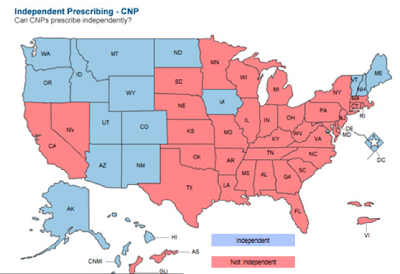
Seventeen states and the District of Columbia allow full prescribing authority for nonscheduled medications to nurse practitioners (see chart below), which means they do not require a signed agreement with a physician. Note that no Southern states allow nurse practitioners to work independently.
A recent report by Deloitte Consulting estimated that the state needs 3,790 more doctors just to meet current demand, which means this is what is needed even before considering the health law or Medicaid expansion. The report says that unlike the need for nurse practitioners, which is balanced between rural and urban populations, the state’s doctor shortage occurs mostly in rural areas; the need was 61 percent rural in 2012 and is forecast to be 63 percent rural as Medicaid also expands.
The state needed 183 primary care physicians in 2012, and will need about 284 by 2017. The neediest counties are Bullitt and Spencer, which are close to Louisville. The need is heavily concentrated in the eight southwest border counties, and with Medicaid expansion, it will increase by 42 percent, says the report.
It’s clear that large gaps appear in Kenucky’s health-care workforce in Kentucky, particularly in rural areas, the Deloitte report says. A more detailed look at the county level is needed to determine the true workforce capacity issues, and can be done by provider type through an interactive tool the firm developed by clicking here.
The need for nurse practitioners in 2012 is relatively low compared to other groups — 148, or 5 percent of the current supply, says the report. However, “If 6 percent of the current [NP] population were added to the current PCP [primary care provider] supply, the entire PCP gap could be addressed,” the Deloitte report says. (NPs are generally referred to as advance practice registered nurses, or APRNs, as indicated on this map.)
To help address this overall provider shortage, Deloitte made 11 recommendations to the state, one of which included authority for nurse practitioners to prescribe less risky drugs without an agreement with a physician. This has been the issue debated by NPs and doctors at the legislature. The report says loosening collaborative agreements could do a lot to address the need for primary care. Giving nurse practitioners more authority has many benefits, including the fact that nurse practitioners who would be able to work more independently may be more likely to set up practice in rural areas.
Some other recommendations in the report include creating support programs for small practices in rural and under-served areas; considering limits on medical malpractice awards; expanding regional rural health tracks to get more new doctors to rural areas and keep them there; and increasing health-care degree and residency capacity across the state.

