Kentucky, insurance companies are applying lessons learned in state’s hurried transition to managed-care Medicaid
Kentucky Health News
Gov. Steve Beshear rushed to transplant Medicaid into a new bed called managed care, hoping the new medium would save money and improve health, but his administration didn’t take time to condition the soil, fertilize the ground or oil the machinery in 2011. This month, managed-care company Kentucky Spirit proved to be the self-plucking bad weed, fleeing the state as it cited unbearable costs.
Kentucky’s hurried transition to Medicaid managed care has been anything but smooth for many doctors, hospitals and other health-care providers. They have complained about late payments and burdensome reimbursement processes.
It’s also not been smooth for the state or the managed-care firms, which are subsidiaries of insurance companies. There have been court battles, tension-filled negotiations, dropped contracts, allegations of a contract breach and now the departure of Kentucky Spirit, pushing its 125,000 clients to one of the other two companies operating outside the Louisville region.
Most important, patients have suffered from the rapid switch and ensuing wrangles. They complain that prescriptions previously covered by the old “fee for service” system are now denied as not being”medically necessary” by managed-care firms, which the state pays a set fee per person. Patients in rural areas complain because they must drive long distances to find providers in their Medicaid company’s network.
But there have been improvements in delivery of health care, particularly in the areas of vaccinations and other preventive services, says the state Cabinet for Health and Family Services. Those include a 33 percent increase in flu vaccinations and an increase in immunizations for children, more well-child visits, increased smoking-cessation consultation, and more than a 50 percent increase in diabetes testing, cabinet spokeswoman Jill Midkiff said.
State and companies made some missteps
Amid those encouraging signs for the future, most of the news about managed care in the past 10 months has been about Kentucky Spirit’s potential departure which occurred July 6. The cabinet is preparing legal action to seek damages from Kentucky Spirit for abandoning its contract; the company, a subsidiary of St. Louis-based Centene Corp., says it didn’t break the contract and took every step possible to make a smooth and orderly transition. The state Court of Appeals ruled that Kentucky Spirit could end its contract without a two-month transition period for patients because the state had plenty of time to make arrangements for the company’s departure.
It’s not clear that the state can recoup damages, or lost taxpayer money, from Kentucky Spirit, though it is having to pay the other two companies more because Kentucky Spirit was initially the low bidder for a managed-care contract. CoventryCares and WellCare of Kentucky are paid an average of about $100 more per month per Medicaid patient.
When Kentucky Spirit first threatened to leave in October 2012, it said it was losing money due to “faulty data” the state provided during the bid process. The two other companies received the same information.
“There were no flaws in the state’s data book,” CoventryCares CEO Michael Murphy told Kentucky Health News. But he said the companies miscalculated because the data book didn’t refer to retroactive payments. That led to a loss of $50 million for Coventry in the first quarter of 2012, he said. Now, he added, the company has a greater understanding of the system.
WellCare, asked if the state provided faulty data, did not answer as definitively. “Medicaid programs are expansive and complex, and it is not unusual for any state to provide data during a RFP [request for proposals] process that may have anomalies or other issues that could negatively impact rates if left unaddressed over time,” said Mike Minor, president of the firm.
Schedule seemed politically influenced
Both companies said the state’s transition to managed care was rapid and taught difficult lessons. That raises questions about whether haste made waste. Kentucky Spirit blames the state for its losses, and providers blame managed care companies for reimbursement issues, but evidence continues to clearly indicate two problems: too little time and money.
The state has been using managed care in the Louisville region through the not-for-profit Passport Health Plan since the late 1990s, and had long considered expanding it to other parts or all of the state to save money as Medicaid costs burgeoned, especially during the Great Recession.
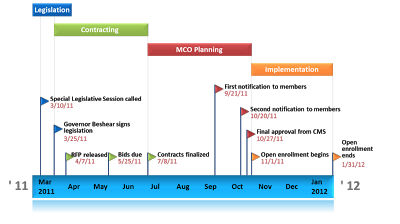
Gov. Steve Beshear proposed statewide managed care in the budget he gave the General Assembly in early 2011, called a special legislative session to authorize it in March 2011, and signed the legislation on March 25 of that year. The state requested proposals from managed-care companies two weeks later, and bids were due less than two months later.
Contracts were finalized July 8 but implementation was not scheduled until Oct. 1. It was delayed until Nov. 1 “at the insistence of the Kentucky Hospital Association,” which “asserted more time was needed for hospitals to negotiate contracts with plans,” says a University of Kentucky report published last year and funded by the Foundation for a Healthy Kentucky.
“Several informants told us that they believed that the upcoming election
for Kentucky’s race for governor was a primary contributing factor in the rapid
implementation timeline,” the report says. “Beshear’s
office saw the closing of this gap as a major issue that needed to be addressed
before the November election,” which was held Nov. 8. That effectively delayed most publicity about complaints regarding implementation until after the election.
“There is no doubt that the commonwealth’s rapid transition from a Medicaid fee-for-service program to a managed-care program raised a number of unforeseen challenges,” said Minor, of WellCare.
“Certainly, the short timeframe . . . made for a difficult transition,” said Midkiff. “Despite the negative portrayal of the managed-care companies, much progress has been made . . . and we expect that progress will continue.”
 |
| Implementation timeline from UK’s Medicaid managed care report |
In October 2012, the managed-care companies continued to be dissatisfied with their fees, claiming they were inadequate to provide quality care, says the UK report. In January 2013, the state gave CoventryCares and WellCare 3 to 5 percent rate increases.; Kentucky Spirit asked for 21 percent, Murphy said, but got only 1 percent.
Murphy said the state had reduced rates below those established by the federal Centers for Medicare and Medicaid Services. “We want to establish base rates for primary care services that we hope the state will continue,” he said.
Minor said, “While there were legitimate prompt-pay issues during the first six months of implementation of Medicaid managed care, we are now well past those issues.”
Looking ahead
Murphy said some of CoventryCares’ initial failures were due to the company’s lack of understanding, and it has found Health and Family Services Secretary Audrey Haynes and her actuaries very cooperative and transparent, helping improve the system. “CoventryCares had to first figure out the problems going on with providers and payments. We had to understand the risks we had, and things have settled down quite a bit, especially regarding the pre-authorization process,” he said. “We’ve stopped the bleeding.”
Murphy said health-care providers will bear the burden of Kentucky Spirit’s departure. To resolve issues faced by providers even before that, the cabinet has held regional forums across the state. Reception at the forums has been positive, and providers have been grateful for the opportunity to address any problems or complaints they have with the cabinet and Medicaid staff, said Midkiff.
Some providers still complain, saying that they should not have to meet with managed-care and state officials to receive payment for services already provided to Medicaid patients.
Starting in January 2013, primary care providers were supposed to be paid Medicare rates for Medicaid services over a two-year period, but some providers have yet to see that rate increase. Murphy said Coventry is planning to pay the increased rates as soon as the state’s application is approved by federal officials.
Murphy said managed care should not be about the money, but about the member. He said primary care is at the core of improved health outcomes. Minor said WellCare has also made it a goal to establish relationships with primary-care providers.
But for those primary-care providers facing financial difficulties in wake of payment cuts, it is about the money because they need it to keep their practices open.
One of providers’ latest complaints is CoventryCares’ recent limit on dispensing certain prescription pain killers, to a 15-day supply. The move was made “to curb the manipulations going on with opioid painkillers,” said Russell Harper, the company’s director of government relations.
Murphy said, “It’s not everybody, but there are physicians that don’t want to engage in health care.” He acknowledged that the prior-authorization process between doctors and pharmacists can be a hassle, but it’s just another facet of managing the health care of Medicaid patients. That, and saving money, are what managed care is all about.
Very good article! -Sarah Vickers