Common blood thinner Coumadin is causing deaths and injuries in nursing homes, prompting calls for more regulation
The analysis only includes Coumadin injuries that are reported, but “studies suggest there are thousands more injuries every year that are never investigated by the government,” Ornstein writes.
Coumadin is a popular preventer of heart attacks, strokes and blood clots, but patients who use it must be carefully monitored. “Too much, and you can bleed uncontrollably; too little, and you can develop life-threatening clots,” Ornstein warns.
 |
| Graphics by The Washington Post |
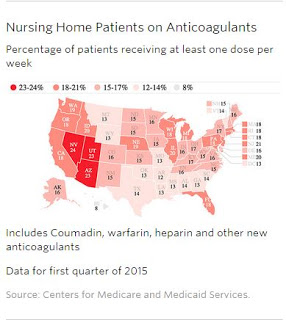
It is one of the most used drugs in Medicare’s prescription-drug program, with one in six of the nation’s 1.3 million nursing-home residents taking an anticoagulant, mostly Coumadin or its generic, Ornstein reports.
Improper administration and poor monitoring of patients who use Coumadin can cause serious harm or even death. Ornstein tells of several such nursing-home cases, each stemming from a different type of error:
“Dolores Huss, an 89-year-old grandmother of eight, died from internal bleeding after a San Diego facility gave her an antibiotic that multiplies the effects of Coumadin, then didn’t alert her physician that she needed additional blood tests to measure how long it was taking her blood to clot.”
“Shirley Reim, recovering from hip surgery, was hospitalized with blood clots in her legs after a Minnesota nursing home failed to give her Coumadin for 50 days in a row and also didn’t perform the blood test ordered by her doctor. She suffered permanent damage.”
“Loren Peters arrived in the emergency room in October 2013, bruises covered his frail body, and blood oozed from his gums. The 85-year-old had not been in a fight or fallen down.” Instead, he had been given too much Coumadin and “no one at the nursing home conducted the blood test needed to see the effect Coumadin was having, even as bruises spread across his body over a two-week period.”
Instead, individual cases are investigated as they come to the attention of CMS and depending on the circumstances, “CMS will issue “immediate jeopardy” citations, fine them or threaten to cut off federal funding if quick action isn’t taken,” Ornstein writes.”More commonly, though, homes are not fined and are simply asked to correct the problems and put policies in place to keep them from happening again,” according to the analysis.
“Last year, the Department of Health and Human Services identified Coumadin and other anticoagulants as one of the drug categories most frequently implicated in “adverse drug events,” calling on government agencies to work on solutions,” Ornstein reports. In a statement, CMS, which is part of HHS, said “it is raising awareness of such events, training its inspectors to do a better job at identifying them and working with nursing homes to prevent them.”
There are newer anticoagulants, like Eliquis, Pradaxa and Xarelto, that don’t require regular blood tests and don’t have to avoid certain foods, but they come with their own risk, like gastrointestinal bleeding,which makes doctors reluctant to use them on seniors.
Coumadin requires the coordination of doctors, nurses, pharmacists and laboratories, which makes nursing homes the “perfect setup for bad things happening,” Jerry Gurwitz, chief of geriatric medicine at the University of Massachusetts Medical School, told Ornstein.
Gurwitz wrote about this problem in the 1990s and says since, “very little, unfortunately, has changed.”
Ornstein notes that “federal inspection reports repeatedly cite the same types of problems: patients not getting the drug as ordered, or given the wrong doses, or given without a doctor’s order.”
Increased training doesn’t seem to make any difference, prompting some to call for federal regulations.
“A report published last year in The Consultant Pharmacist journal found that 12 New York nursing homes given tools to improve how they handled patients on Coumadin — including staff education programs — largely failed to improve their management of the drug,” Ornstein writes.“Improvements were not seen despite active intervention,” the report’s authors wrote. “If long-term care facilities are unable to voluntarily implement necessary improvements, then regulatory changes may be necessary to assure patient safety regarding anticoagulant use.”
David Gifford, senior vice president of quality and regulatory affairs at the American Health Care Association, told Ornstein that “Coumadin errors can’t be viewed in isolation.” and said that the association has introduced a quality initiative that covers all types of errors, including those involving medications.
Some long-term care associations say CMS should work with the industry to change its practices including looking their current policy of reviewing each case individually and its discipline policies, Ornstein reports.
Another concern is not to discourage doctors from prescribing Coumadin.
“It may be distorting a little bit to look at the immediate jeopardy outcomes [cited by regulators] without looking at the overall population that’s on it and needs to be on it,” Cheryl Phillips, senior vice president of public policy and advocacy at LeadingAge, an association of nonprofit senior service organizations, told Ornstein. “In fact, to not put people on blood thinners is a huge risk and in many cases malpractice.”
Click on ProPublica’s Nursing Home Inspect tool to compare more than 60,000 nursing-home inspection reports.