In study of how 15 states dealt with health reform, Kentucky was by far No. 1 in cutting the number of unpaid hospital stays
By Melissa Patrick
Kentucky Health News
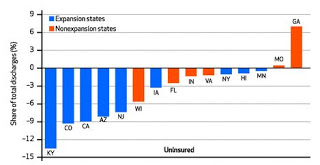
Kentucky hospitals had the biggest drop in non-paying patients among 15 states in an ongoing study of the effects of Medicaid expansion under federal health reform.
Kentucky showed a decline of 13.5 percent in unpaid
hospital stays in just the first six months after the 2014 expansion, according
to the study at the University of Michigan. The next highest state was Colorado, with 9.1 percent.
Hospitals in states that expanded Medicaid, like Kentucky, are taking care of more patients with health insurance, and thus have seen an increase in payments for their care. The study looked at nine of those states and six that did not expand Medicaid coverage, based on data available at the start of the study. Four of those six also saw decreased in unpaid hospital stays, but less than most of the expansion states.
Overall, hospital stays by uninsured patients went down 50 percent, and stays by people with Medicaid went up 20 percent, between the end of 2013 and the middle of 2014, a University of Michigan news release says.
That is what the Patient Protection and Affordable Care Act intended, giving hospitals a chance to recoup some of the cost of care they have long provided at no cost, the release said.
Kentucky has added about 400,000 people to its Medicaid rolls since it expanded the program to those with incomes up to 138 percent of the federal poverty level. The previous limit was 69 percent.
Republican Gov. Matt Bevin has repeatedly said Kentucky can’t afford to pay for this expanded population. He has appointed Mark Birdwhistell, a University of Kentucky health executive and former state health secretary, to help him design a new Medicaid plan that will save money while providing needed care.
If the plan reduces the number of Kentuckians on the Medicaid rolls, that is likely to increase the amount of uncompensated care absorbed by Kentucky’s hospitals. That would increase the financial pressure on hospitals at a time when the federal government will “ratchet back the federal funds that some hospitals get to make up for some of the cost of caring for the uninsured,” the release notes.
The study, published in the January issue of the journal Health Affairs, looked at Medicaid expansion states Arizona, California, Colorado, Hawaii, Iowa, Kentucky, Minnesota, New Jersey and New York. The non-expansion states were Florida, Georgia, Indiana, Missouri, Virginia and Wisconsin.
The study found that hospitals in states that did not expand Medicaid “continued to experience the same or even higher demand for care from people without insurance.” Georgia, a non-expansion state, saw a 7 percent rise in uninsured hospital stays in the first half of 2014.
In Wisconsin, which had a drop in unpaid stays larger than some of the expansion states, there was a “welcome mat” effect, which prompted enrollments from people who had been eligible but not on the program but became aware of it because of the reform law. In Kentucky, that is called the “woodwork effect,” as in “people coming out of the woodwork.”
