Many Americans, including those on Obamacare plans, can’t afford their health-insurance deductibles, studies show
 |
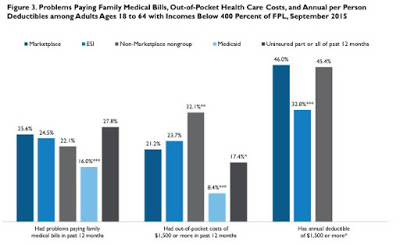
| Graph: Urban Institue’s Health Reform Monitoring Survey |
Nearly 25 percent of Americans surveyed last September who had coverage through employer plans, the Affordable Care Act, or individual plans outside health-insurance exchanges reported problems paying family medical bills in the previous 12 months, according to the Urban Institute‘s Health Reform Monitoring Survey. That compared with 16 percent of people on Medicaid and 27.8 percent of the uninsured.
The Kaiser Family Foundation also found that people on Medicaid or policies bought through the federal or state exchanges, also called marketplaces, couldn’t afford their deductibles. This 2016 focus group study of 91 low-income Medicaid and exchange-plan enrollees in six cities found that “all reported that they had trouble affording some aspect of their current coverage, including premiums, deductibles, and/or co-payments.” It also found that “nearly all marketplace participants” said they had received unexpected bills for services they thought were covered, and fear of this often led them to forgo care.
The latest Kentucky Health Issues Poll found that affordability is also a problem in Kentucky, with 28 percent of Kentucky households having at least one person who reported struggling to pay their medical bills in the previous 12 months. This rate was about the same as in 2014 and didn’t vary much between those with insurance or without insurance. In addition, the poll found that 20 percent of Kentucky households did not get the medical care they needed, or delayed care because of cost in the past 12 months.
This lack of affordability also affects health-care providers. Meyer reports that the chief financial officer for Community Health System told analysts at the first-quarter earnings report meeting that the fourth quarter of 2016 will be his company’s best quarter, because patients will have hit their insurance deductibles and only then be able to afford needed care at their facilities.
“As individuals take on high deductibles and higher co-pays, they are essentially taking on insurance risk they can’t necessarily afford,” Trevor Fetter, CEO of Tenet Healthcare Corp., told Meyer. Fetter told Meyer that his company now focuses on helping patients understand how to pay their bills, “including pressing for cash payments at the point of service.”
What are the presidential candidates saying?
Meyers writes that Democratic front-runner Hillary Clinton offers the most help for those who can’t afford their high deductible. She says she “would require health plans to: cover three annual visits to a doctor for illness without applying the deductible; give insured people a $5,000-per-family refundable tax credit for out-of-pocket costs exceeding 5 percent of their income; cap out-of-pocket costs for prescription drugs; bar providers and insurers from charging patients out-of-network bills for services received at an in-network hospital; and strengthen states’ authority to block excessive insurance premium increases.”
“Vermont Sen. Bernie Sanders, Clinton’s Democratic opponent, wants to eliminate premiums and cost-sharing entirely by establishing a tax-funded, government single-payer insurance program covering the full range of healthcare services, including long-term care,” Meyer writes.
“Donald Trump, the presumptive Republican nominee, has released a seven-point health policy agenda that doesn’t directly address out-of-pocket costs. It would offer households a tax deduction for buying coverage, expand health savings accounts, and let insurers sell plans across state lines,” Meyers writes.
Meyers calls the issues surrounding high deductible plans and high prescription drug costs “the domestic policy elephant in the room,” and says these issues are not getting enough attention.