Survey of low-income Kentuckians, Arkansans suggests expansion of eligibility for Medicaid is making them healthier
The telephone survey of more than 8,500 low-income citizens of Kentucky, Arkansas and Texas was part of a Harvard University study published Monday in the medical journal JAMA Internal Medicine. The researchers found that low-income people in Kentucky and Arkansas, which expanded Medicaid eligibility to 138 percent of the federal poverty level, appear to be healthier than their peers in Texas, which did not expand Medicaid access.
The surveys of Medicaid-eligible people found that those in Arkansas and Kentucky were 4.8 percent more likely than their peers in Texas to say they were in excellent health in 2015.
That difference was bigger than the 2.4 percent difference found in the 2013 and 2014 surveys, which is to be expected because “significant impacts of Medicaid expansion may take several years to unfold,” the researchers wrote.
“After two years of coverage expansion in Kentucky and Arkansas, compared with Texas’s non-expansion, there were major improvements in access to primary care and medications, affordability of care, utilization of preventive services, care for chronic conditions, and self-reported quality of care and health.” But they cautioned, “It remains to be seen whether the modest changes detected in our study will lead to subsequent improvements in objective measures of population health.”
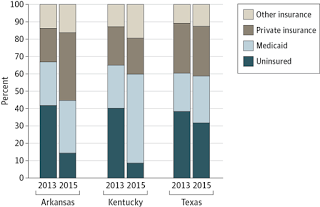
 |
| Results from surveys of people with incomes below 138 percent of federal poverty line. Arkansas expanded Medicaid through private insurance. Texas has not expanded it. (JAMA Internal Medicine) |
The survey also found that people in Kentucky and Arkansas were more likely to have a doctor and a place to go for care than in Texas, Margot Sanger-Katz reports for The New York Times. They said they were more likely to have their chronic disease treated, and that they were more likely to have received screening for high cholesterol or high blood sugar, markers for heart disease and diabetes.
Measuring whether people are healthier may sound simple, “but it’s actually pretty tough,” Sanger-Katz writes. While tests can check for high cholesterol or high blood pressure, “a single test may not tell the whole story. It turns out, however, that when you ask people how healthy they are, they do a pretty good job of telling you.”Research shows that people who say they are in poor health are more likely to die soon than those who describe their health as good.
Arkansas’ expansion works differently than Kentucky’s traditional Medicaid expansion in that it helps low-income residents buy private insurance. Either way, greater access to health insurance seems to be creating positive health outcomes.
“What this means is that it doesn’t matter so much how states expand coverage,” Benjamin Sommers, primary author of the study and assistant professor of health policy and economics at Harvard’s School of Public Health, said in a news release. “What matters is whether they expand at all.”
The researchers were quick to warn that the findings were not necessarily generalizable to other states. “Medicaid programs vary widely across states in terms of physician payment, covered benefits, and other features, which means that our results are in some sense a case study of two specific expansion efforts,” they wrote.
Even so, Sommers and the other researchers concluded their study with some advice based on their findings: “As Kentucky and Arkansas reconsider the future of their expansions, our study (along with evidence on the financial benefits to these states of expansion) provides support for staying the course.” Gov. Matt Bevin is expected to formally propose changes to the federal government this month.