By 7-1, public comments in 3rd round on Kentucky Medicaid plan oppose it; suit filed to stop similar work requirements in Arkansas
By Melissa Patrick
Kentucky Health News
When the third round of public comments on Kentucky’s proposed Medicaid plan ended at 11 p.m. EDT Saturday, Aug. 18, more than 11,500 people had posted their views online, and, much like twice before, more than 80 percent of the commenters opposed the changes.
Kentucky Health News took a random sample of 200 comments and found that 175 either firmly opposed the changes or made positive comments about Kentucky Medicaid as it exists, and 25 opposed it: 87.5 percent to 12.5 percent, or 7 to 1. The sample’s margin of error was plus or minus 6.9 percentage points. Click here to view a summary of all of the responses.
The federal Centers for Medicare and Medicaid Services re-opened the plan for comments after a federal judge vacated it just days before it was set to start on July 1. The judge said the U.S. Department of Health and Human Serviceshad not adequately considered the state’s estimate that in five years its Medicaid rolls would have 95,000 fewer people with the plan than without it, in large measure for non-compliance with its requirements. Those include work, school or other “community engagement” rules for able-bodied adults who are not primary caregivers.
A CMS spokesperson told Politico in July that the agency re-opened the comments “to better inform any future decision on the demonstration that was remanded back to the department for further review.” Judge James Boasberg’s ruling had specifically criticized HHS Secretary Alex Azar “for disregarding public comments that were overwhelmingly against the plan.”
Robert Pear of The New York Times reports, “Administration officials said they could sidestep the ruling by providing a better explanation of the rationale for work requirements.”
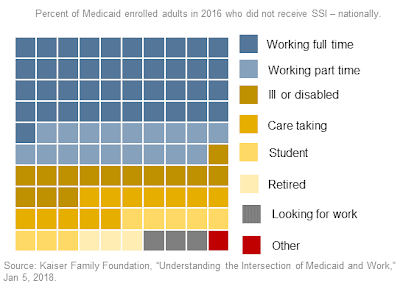
In opposition to the work rules, one commenter cited a Kaiser Family Foundation study and said, “Work requirements would affect a very small percentage of Medicaid recipients, while imposing unnecessary burdens on the rest. Being poor and needing medical care should not require a punitive and demeaning amount of paperwork. I oppose work requirements in the strongest possible terms. Don’t waste any more time fighting what the courts have already deemed a lost cause.”
Many others told how the 2014 expansion of Medicaid had helped them, and voiced their concerns about the possible changes. “I was working, but as a part-time employee I didn’t qualify for the company insurance,” said one who became eligible for Medicaid. “I have several health issues and keeping up with the cost of medicine wasn’t easy. Having Medicaid has been a blessing. I’m now retired and confused about the new health program.”
U.S. Rep. John Yarmuth, D-Louisville, submitted a formal comment opposing the work requirements in the plan, called Kentucky HEALTH for “Helping to Engage and Achieve Long Term Health.”
“While there are certainly benefits to employment, work requirements have long been proven ineffective in meeting this goal, and are particularly cruel given the challenges many low-income Kentucky families face in the job market,” Yarmuth wrote. “In fact, as was recently reported in The Wall Street Journal, “(taking) medical care away from low-wage workers in unstable jobs is not only ineffective in promoting employment, it may be counterproductive, since losing access to regular treatment can make it harder for people with serious health needs to look for and keep a job.” Taking health care away from 95,000 people, as Kentucky HEALTH would do, would not make them healthier or increase their employment prospects.”
The liberal-leaning Kentucky Center for Economic Policy‘s 13-page letter said it spoke directly to the federal court’s ruling, “namely that the proposed changes contradict the purpose of the Medicaid program, which is to provide health coverage to those who cannot afford it. The waiver would result in unacceptable coverage losses, and therefore should be rejected.”
Another in support of the changes more bluntly echoed the “skin in the game” arguments that Gov. Matt Bevin has used: “Hell yes it needs to be approved. Why would someone who is able to work be allowed to sit home and not do anything and collect welfare and be eligible for Medicaid? Yes, Approve this. Kentucky cannot continue to fund the cost of the Medicaid program.” In support of Kentucky HEALTH, one health-care worker wrote, “I think KY should be allowed to institute work requirements and any other requirements for Medicaid recipients they deem necessary. As a provider in Kentucky I see Medicaid recipients every day who are abusing the system by qualifying for benefits when they really should not. Our current system has become a lifestyle instead of a helping hand. I have to work to pay for my extremely expensive health care (and) I can’t find a reason that an able bodied person should not have to show some effort for their free health care.”
Many of the comments opposing the changes were collected and posted by Kentucky Voices for Health, a coalition of lobbying groups supporting the status quo, reports WUKY, the University of Kentucky‘s radio station. It quotes outreach and education director Angela Koch as saying, “Medicaid waivers are supposed to be innovative. They are supposed to change the way Medicaid works for the better, and this waiver does the opposite. It breaks Medicaid.”
Supporters of the mandate counter that finding employment will help people move out of poverty and improve their health in the long run.
Kentucky HEALTH would require able-bodied adults who are not primary caregivers to work, attend school, take job training or volunteer 80 hours a month, or enroll in a drug-treatment program if appropriate. It also includes small, income-based premiums and lock-out periods for non-compliance.
Jill Hunter, Kentucky’s acting Medicaid commissioner, told Darla Carter of Insider Louisville that she didn’t know when the state would hear back from CMS, but said, “I know that we’re ready; just let us know when it’s time.”
CMS has also approved work requirements for Medicaid in Arkansas, Indiana and New Hampshire. Seven other states, Arizona, Kansas, Maine, Mississippi, Ohio, Utah and Wisconsin, have applied for permission to implement them.
Two of the same groups that filed the lawsuit for Kentucky Medicaid recipients, the National Health Law Program and the Southern Poverty Law Center, have joined with Legal Aid of Arkansas to file a similar federal lawsuit to block the Medicaid work requirements in that state.
In June, Arkansas was the first state to implement Medicaid work requirements and new state data shows that “thousands of Arkansans may lose Medicaid without even realizing the rules have changed,” according to an analysis from the Georgetown University Health Policy Institute.
The institute says that out of about 15,000 people who were expected to record their work activities, 5,426 are in their second month of noncompliance and only 844 had satisfied their reporting requirements, Those who fail to document 80 hours a month for three months can be kicked off the program.
Because of the similarities in the Arkansas and Kentucky cases, the Arkansas suit was assigned to U.S. District Judge James Boasberg of Washington, D.C., who has retained jurisdiction in Kentucky’s case.