Virus has spread too much for contact tracing to contain it, but tracing can still help, especially if more people would cooperate

By Lisa Gillespie
Kentucky Health News
In wide swaths of Kentucky, tracing the contacts of people with the coronavirus is no longer preventing its spread, because the spread has become too wide. Instead, it is, at best, slowing the disease rate. And many people don’t cooperate with the contact-tracing process.
That’s according to several local health department officials, including Roanya Rice. She’s the public health director at the North Central District Health Department, which includes Spencer County, where over 10% of residents have tested positive for the virus, as of last week.
“It’s not a situation now that we can contact-trace our way out of,” Rice said. “The window of opportunity to contact-trace to eliminate the spread has come and gone.”
Some people don’t welcome contact tracing, which usually includes an official request that they isolate for 10 days in case they have the virus. Gov. Andy Beshear said this week that there has been a decline in cooperation by people who have been identified as a recent contact or have tested positive..
Lincoln Trail District Health Department Director Sara Jo Best said she and her staff get the feeling that some people who have tested positive don’t want to provide a list of their recent contacts.
“I feel like there are cases that are not being 100 percent truthful in their contacts,” said Best, who is based in Elizabethtown. “I think they’re intentionally leaving some of those off, because people don’t want to be quarantined.”
Beshear said some people reached by contact tracers are unresponsive or don’t self-isolate as requested.
“They could lead to another spike,” he said. “This is a war. Whether we win or lose, how many Kentuckians we lose, it’s all based on the number of battles that we win, or lose. So please, don’t get tired. Let’s pick it up. Lives, lives depend on it.”
Local health officials say most people cooperate when a contact tracer reaches out. They say they have only rough and unscientific estimates on the percentage of people who are not cooperative, because the state only recently provided a uniform platform for health departments to track cases. Department directors, when pressed, estimated noncompliance between 2% and 40%.
Barren River District Health Department Director Matt Hunt said the people who are not cooperative in his eight-county region are mainly those without symptoms. His district includes Barren County, where more than 10% of residents tested positive for the virus Aug. 15-21, the most recent week of the White House Coronavirus Task Force report.“We do have some that deny the test results, [say] that it can’t be, [they] don’t have symptoms,” Hunt said. “Those are typically asymptomatic individuals. Those are difficult conversations to have.”
Others have used a “critical worker exemption” to refuse quarantine after a high-risk exposure. State Health Commissioner Steven Stack announced Wednesday, Aug. 26, that he had eliminated the exemption for workers in food, health care, energy and other critical industries, saying it had become “fairly distorted . . . Health departments are finding all sorts of people are claiming they’re critical infrastructure workers.”
Meanwhile, health department directors across the state say the virus has spread so much within communities that contact tracing is not containing the spread of the virus. Lexington-Fayette County Health Commissioner Kraig Humbaugh said that’s partly because of how the virus works; the key time to get folks to quarantine is when they start to show symptoms. But many never have symptoms.
“Normally [the contacts] are infectious a couple of days before they even start to show symptoms, if they show symptoms, and then 25 percent of them don’t,” Humbaugh said. “So you’ve got all those people that are also potentially infecting others in the community. It just kind of builds on itself. It is so much easier for this strategy to work when we’re in the containment phase.”
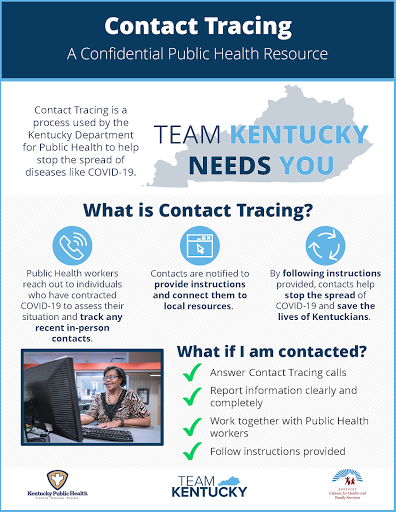 |
| Department for Public Health graphic; for a larger version, click on it. |
Kentucky has funds to hire 700 contact tracers and has hired 550, with at least one in every county. That leaves room for 150 spots. Mark Carter, the state official leading contact-tracing efforts, estimates those new hires will be made by or around mid-October, depending on the spread of the virus.
“The Department for Public Health assessment of tracing state-wide is that we have sufficient tracers,” Carter said. “The primary issues have been in masking and social distancing; that places a burden on tracing. So, I think it would be fair to say tracing is helpful, but by itself it cannot stop the spread. I do agree that certain districts are in a mitigation phase,” not a containment phase.
With many Kentuckians ignoring the mask mandate and social-distancing guidance, which is difficult to enforce, health officials say contact tracing is the actionable thing health departments can do to fight the virus without a vaccine.
But the funding for tracers runs only through December, and it’s unclear whether Congress will provide more. Hunt, with the Barren River health department in Bowling Green, is hoping the money doesn’t run out before he needs the help the most.“I want to try to stay two to three steps ahead,” Hunt said. “If I see a spike, like instead of having 25 or 30 to investigate a day, it jumps up to 75, then I’ll start to think about, okay, we need to bring more people in.”
Contact tracing does play a role in fighting the virus, even if it’s not containing spread. Public Health Director Clayton Horton of the Green River District Health Department in Owensboro said at the very least, tracers provide important education about the virus. And it can be critical for Kentuckians who were already living in relative isolation.
“We have people that are in isolation that don’t have friends and family that can help support them,” Horton said. “We have people that have real needs in terms of food and medicine, and we’re able to help with that, and if we weren’t there, they certainly would break their isolation and put others at risk of becoming infected.”
Another issue that may add to noncompliance is the changing guidance from the federal Centers for Disease Control and Prevention about who should be tested. Horton said one recent change, already walked back, has already created confusion and resistance to the department’s guidance.
“We had contacted them to say, you’ve had contact with someone that was infected,” and advised them to quarantine, Horton said. “And they said, ‘Well, I just saw on the CDC website this morning that I don’t need to do these things,’ and it was just kind of a misinterpretation.”
CDC now says people who have been exposed but have no symptoms “may consider testing.” Kentucky officials are still recommending that such people get tested, because people without symptoms can still spread the disease.
Non-existent numbers
By the start of September, the majority of state health departments should be using new technology to track covid-19 data, called the Contact Tracing and Tracking system. Data on the virus now, other than the raw numbers of who has tested positive, are almost nonexistent.
“As of next Monday (8/31), all but one local health department will be CTT; at that point we will be in a much better position to be able to report this data,” Carter said. I would say that by the end of September or mid-October, we will have some usable data from the system.”
At the start of the pandemic and even now, many departments were using paper charts to log cases; others were using internal systems.
Most health department directors said they’ve just been trying to keep on top of new cases and contacts. There hasn’t been time for analysis.
That’s a real disadvantage, said Best, with the Lincoln Trail district. She wants to know the number of contacts who test positive for the virus. She wants to know the percent of people who never respond to their calls, and those who initially are cooperative but then no longer answer calls or emails. She wants to know not just her district’s own numbers, but also the state-wide average.
“If I know that of one thousand contacts, 20 percent of those are probably going to convert to a positive, that helps me plan,” Best said. “Or if the state’s average is 20 percent, and my average is 40 percent, maybe I need to re-look at how we’re educating people on isolation and quarantine. I might need to evaluate what I’m doing because it’s not it’s not effective. It gives you kind of benchmarks like that when you’re looking at data.”
And this information might just make contact tracing a stronger tool.