‘Prostate cancer is to men as breast cancer is to women,’ survivor writes for National Prostate Cancer Awareness Month
By Steve Ranson
Prostate cancer is to men as breast cancer is to women.
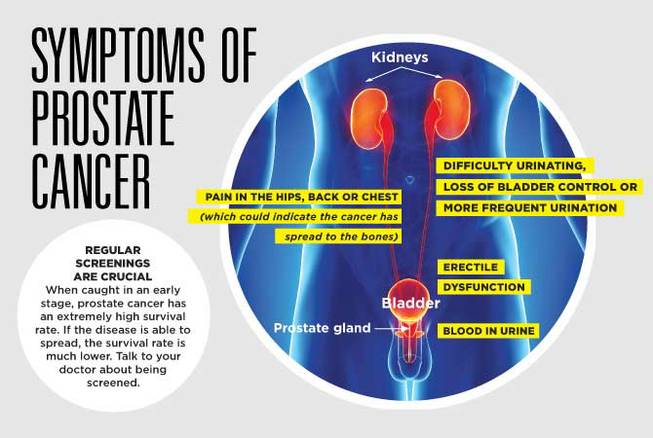
The second-leading cause of cancer deaths in men comes from a small gland located between the bladder and the penis. If not monitored or treated, prostate can be a killer. Likewise, the No. 2 cause of cancer deaths in women is breast cancer. So what’s the difference? Over the years, more awareness has been directed at breast cancer screening than with the prostate gland. Therefore, with September being Prostate Awareness Month, let’s put the spotlight on this type of cancer.
I’m one of those statistical males where prostate cancer will affect one out of nine men in their 60s. I began screening about every 18 months to two years when I was in my 50s, and then about every year to 18 months after I entered my 60s.
An abnormal PSA or prostate-specific antigen found in the blood alerts physicians that prostate cancer may exist. During the past six years, my PSA slowly climbed from a 3.18 in 2014 to 6.36 in 2017. In 2019, the PSA more than doubled to 16.57, causing my general practitioner to refer me to an urologist. Other warning signs began to develop during the first seven months. I had frequent urges to urinate, but the stream was weak. Occasionally, blood would appear in my urine. Sometimes, I would stand over the toilet, straining to empty the bladder.
My urologist Dr. Brian Montgomery saw me in late August 2019 and quickly re-ordered another PSA. It returned with a score shy of 17.
“The higher the PSA, the more likely prostate cancer,” he said, reviewing the latest result with me.
A month later, Dr. Montgomery completed a core biopsy of the prostate by taking samples from 12 areas. When he presented the results to me two weeks later, I had the presence of cancer in two quadrants, the left base and left lateral apex. Dr. Montgomery’s attention focused on the left later apex, which measured the adenocarcinoma — cancer forming in mucus-secreting glands —up to 16 mm in its greatest dimension and occupying 95% of the surface area.
Furthermore, Dr. Montgomery said the pathologist issued a Gleason grading score of 8, which means I have a high-grade legion than can spread more quickly than scores half that.
The left base showed adenocarcinoma took up only 5%, but the Gleason score came in at 6. Based on my PSA, however, Dr. Montgomery said he expected to see the adenocarcinoma in more than two quadrants.
“It’s all statistics with many different results,” he said.
One test remained before Dr. Montgomery offered his final decision on treatment. A bone scan using criteria based on National Comprehensive Cancer Network guidelines determined if the cancer had spread beyond the prostate to another organ or the bones.
“If you’re metastatic, that basically means high risk,” he pointed out, “but your imagining shows it has not spread.”
Dr. Montgomery said I was very fortunate not to have the cancer in more than two quadrants. Statistically, he said the prognosis shows I have a good chance to beat this disease and there’s an 80% chance I will not have a reoccurrence of prostate cancer.
The treatment: Based on all the tests and the Gleason scores, I was deemed a good patient for receiving radiation treatments instead of having a radical prostatectomy where the prostate and surrounding tissues are removed.
The next step: Dr. Montgomery implanted three radioactive seeds into my prostate that would accurately guide radiation beams to not only the affected quadrants but also the entire prostate.
Dr. Gary E. Campbell, a radiation oncologist with more than 37 years experiences, oversaw the next step with me receiving 43 radiation treatments over three months. The last session on June 1 ended the numerous 128-mile round-trip journeys from my hometown to the center. Willing to answer any questions thrown at him, Dr. Campbell works with his team to develop a tailored plan for each patient.
“We want to take away the fear. It’s scary. Anybody would be scared,” Dr. Campbell said of patients facing radiation treatment.
As the treatments progress, patients begin to feel more relaxed and confident. Seeing and talking to the staff on each arrival seemed like the beginning of the popular television sitcom Cheers … where everyone know your name.
The 43 radiation treatments I received give a higher percentage of killing most cancer cells. Dr. Campbell said statistically, out of hundreds and hundreds of patients, he can tell how they will do with their treatment plans. Chemotherapy, however, is used for advanced prostate cancer and administered on the center’s main floor.
Dr. Campbell also said radiation will work on both the prostate and the tissues associated with the prostatectomy, and since The Carson Tahoe Cancer Center is an affiliate of Huntsman Cancer Institute at the University of Utah, he can access their physicians and findings to assist him developing a treatment plan on answering questions.
Based on his 30-plus years as an oncologist, he said the technology has improved, and the treatments are better tolerated by the patients and more successful because of the center’s multi-million dollar treatment machines.
“It’s kind of like the latest and greatest, and it’s very precise. We are able to push the radiation doses which is important,” he said.
With each 20- to 25-minute treatment, Dr. Campbell said his technicians shoot external radiation beams to the area that’s being treated.
Radiology technician Ellen Plewacki said every patient is treated according to information downloaded from a chart to a computer. For every session, the prostate cancer patient like me lies down on a table, and at a computer outside the treatment room, a technician guides the rays at different angles — nine to be exact — at both the affected quadrants and entire prostate.
“Most of the patients have the same setup and procedure,” she said. “It takes about 2 to 3 minutes to identify the internal anatomy needing treatment.”
Based on dose escalation studies, Dr. Campbell said a higher dose provides the best opportunity to eradicate the cancer.
With the end of radiation treatments almost three months ago, I have encountered side effects from swelling in the legs and ankles, urination and bowel-movement problems, restless nights and some tiredness — they should go away. In order to keep the prostate small and to fight any cancerous cells that may be lingering, I receive a Lupron shot every three months. My main complaint with the shot is how it causes hot and cold flashes and mood swings.
Both doctors, however, have repeatedly said the best indicator of how treatments worked is with another PSA … and with a score of 2 or below.
“I would anticipate your PSA will be extremely low,” Dr. Campbell predicted after I finished the treatments.
My first three-month checkup with Dr. Montgomery occurred in late August, and I had the opportunity to see my first PSA result. Bingo! The result came back as a negative .02, meaning there is no traceable sign of cancer left in the prostate.
“Just what I hoped for,” Dr. Montgomery said.
Steve Ranson is editor emeritus of the Lahontan Valley News in Fallon, Nev. He is a former president of the Nevada Press Association and the International Society of Weekly Newspaper Editors.