Kynect open to preview federally subsidized health plans, with more options and bigger subsidies; enrollment open Nov. 1
Cabinet for Health and Family Services map, adapted by Ky. Health News
—–
By Melissa Patrick
Kentucky Health News
Open enrollment for federally subsidized health-insurance coverage beginning in January will be offered through Kynect, the state’s insurance exchange, which is now online for Kentuckians to explore their options.
The revived Kynect will replace the state’s use of the federal exchange, and will have two more insurers in 2022 than this year — and its first vision coverage. It will also offer less expensive coverage to some people, thanks to greater federal subsidies.
Open enrollment on kynect.ky.gov runs from Nov. 1 through Jan. 15 for health insurance coverage beginning Jan. 1.
Gov. Andy Beshear and U.S. Health and Human Services Secretary Xavier Becerra officially launched the reopening of Kynect as the portal for state-managed health care options Friday at an online news conference.
Becerra called Kynect “Kentucky-made, Kentucky-driven and Kentucky-based” and said the advantages of having a state-based marketplace is that it can be tailored to the needs of Kentuckians.
“I don’t think anyone in Washington, D.C., knows the state of Kentucky and its people better than the governor of Kentucky,” Becerra said. “So his team is going to be able to tailor their marketplace to meet the needs of all the different communities rural, urban, poor, middle class, disabled, you name it, they’re going to know where they need to go, and how to go there better than folks in Washington.”
Kynect was re-launched last year on a limited basis, as a one-stop shop for Kentuckians to apply for Medicaid and connect qualified families to other resources, including the Supplemental Nutrition Assistance Program (formerly known as food stamps) and family and child-care assistance programs.
Now, the platform will again allow Kentuckians to access and compare state-managed insurance options, apply for coverage and complete their enrollment all on one platform, which was its original intent when it was created in the governorship of Beshear’s father, Steve Beshear.
“That makes it a lot easier,” said Priscilla Easterling, outreach coordinator for Kentucky Voices for Health, an umbrella organization of lobbying groups that support continuation and expansion of programs under the 2010 Affordable Care Act, which created federal subsidies for qualified health plans.
Easterling said Kynect allows Kentuckians to access just one platform to determine if they qualify for a qualified plan with income-based subsidies, or for Medicaid, in addition to the other services offered on the site.
“As people’s jobs change or their incomes change, it makes it much simpler to be able to move back and forth between Medicaid and the marketplace, without having to go back and forth between the state and the federal” platforms, she said.
Easterling encouraged Kentuckians without coverage to explore their options on kynect.ky.gov — especially those who looked at plans in the past and found them unaffordable.
That’s because the latest pandemic relief bill, the American Rescue Plan Act, increased the subsidies, and most of its provisions will remain in place through 2022. Easterling said people generally saw a 48% savings on their health-insurance plans with the enhanced subsidies, or an average of $75 a month.
“It doesn’t hurt to just check out what your options are and [find out] what’s going to be available for you and your family,” Easterling said. “You might be surprised, but it’s more affordable than you thought and it’s worth looking into.”
Some small additional savings will result because people who buy health plans through the federal site pay a surch`1arge on premiums, which Kynect will not do. Beshear said it will pass along those savings to consumers.
Easterling reminded Kentuckians that Kynectors, who help Kentuckians sign up for health coverage through Kynect, are available for free in every county to answer questions and help people sign up for coverage.
“Kynectors are a priceless resource that everyone should take advantage of,” said Easterling, who is a Kynector. “If you’re nervous about anything, if you’re confused about any of this process, just call a Kynector because they can walk you through it and will be happy to do so.”
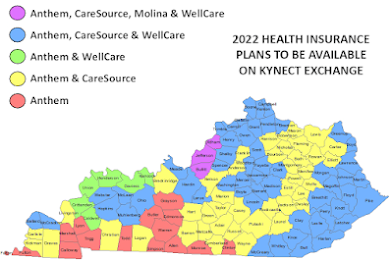
In addition to Anthem’s statewide coverage and CareSource, which is offeing health plans in 100 of the 120 counties, consumers can shop for plans available in select counties from two new health insurers; Ambetter from WellCare of Kentucky, in six western counties, and Passport Health Plan by Molina, in Jefferson, Oldham and Bullitt counties.Fourteen counties will have only Anthem plans to choose from, down from 26 this year. Most are small and rural, but they include Warren County, the core of metropolitan Bowling Green, the state’s third-largest city. Warren and eight neighboring counties also had Anthem as their only choice this year.
And for the first time, Kentuckians will be able to purchase a vision coverage plan through Kynect. VSP Individual Vision Plans will offer enrollees a comprehensive eye exam from an in-network doctor, an eyeglass-frame allowance and lens enhancements, such as progressives.
Kynect was closed in 2017 by Republican Gov. Matt Bevin, who said the site was too expensive to maintain and was redundant. Beshear, a Democrat, said the return to the state-based exchange is expected to save Kentuckians about $15 million a year.
Beshear said Kentucky is getting $650,000 in ARPA funding through the Centers for Medicare and Medicaid Services to help pay for the reopening of Kynect.
He said 280,000 Kentucky adults and 45,000 Kentucky children remain uninsured, and that the goal is to get all of them signed up for health insurance.
Calling Kynect the “gold standard,” Beshear said with Kynect being a one-stop-shop for so many services that provides local supports, a brand that remains strong across the state and the state’s commitment to address any challenges that may come up, “We believe it’s going to be successful.”
Kentucky is among three states to transition from healthcare.gov to their own state-based exchange for 2022 coverage, along with Maine and New Mexico.