Bill would require insurers to cover biomarker testing for cancer; expensive screening tool is ‘cutting edge,’ says sponsor
By Sarah Ladd
Kentucky Lantern
A bill filed Tuesday would require health benefit plans in Kentucky to cover biomarker testing for cancer, with the goal of improving the state’s dismal cancer statistics.
State Rep. Kimberly Poore Moser, R-Taylor Mill, said before filing the legislation, “It’s highly important that we pay attention to science.”
Biomarker testing “is a way to look for genes, proteins, and other substances (called biomarkers or tumor markers) that can provide information about cancer. Each person’s cancer has a unique pattern of biomarkers,” according to the National Cancer Institute.
The American Cancer Society says the testing is “an important step for accessing precision medicine.” It can lead to “improved survivorship and better quality of life for cancer patients.”
The ACS estimates that more than 10,000 Kentuckians will die from cancer this year and 30,000 will be diagnosed with the disease. Kentucky is one of the worst states in the nation for cancer mortality, according to the Centers for Disease Control and Prevention.
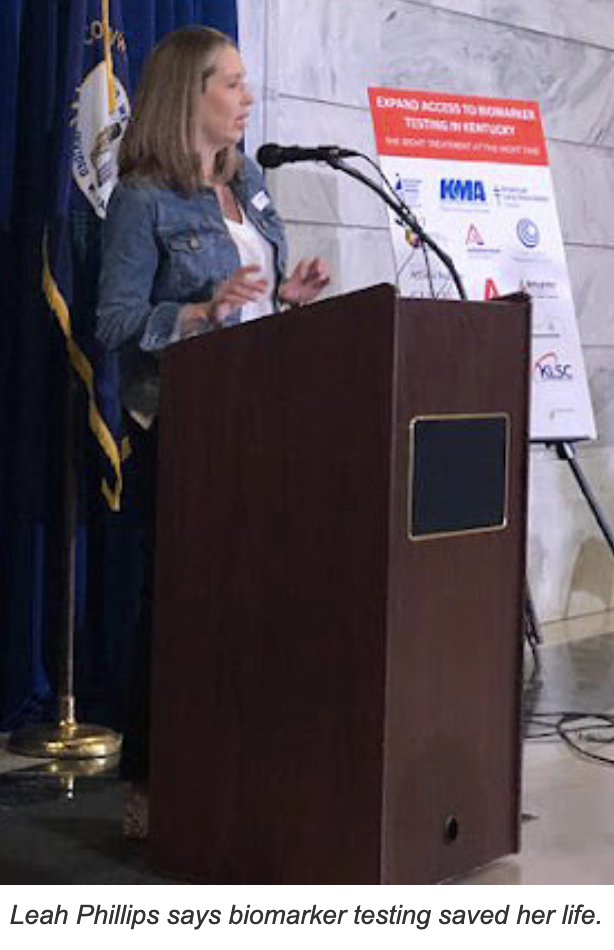
Leah Phillips, a stage 4 lung-cancer survivor from Oldham County, spoke in the Capitol rotunda Tuesday afternoon. Phillips was diagnosed in December 2019. She did not have a smoking background.
She credited biomarker testing with her quality of life.
“If I had not had biomarker testing,” said Phillips, “I would have been treated like a typical cancer patient with lung cancer … and given chemotherapy.”
Biomarker testing showed her cancer was genetically driven, though. She was eligible for a target therapy drug. That treatment provided her “a near normal life,” though it is expensive and not universally accessible.
Dr. Doug Flora is the executive medical director of oncology at St. Elizabeth Healthcare in Northern Kentucky. He said Tuesday, “We’re past the era of chemotherapy for most cancers.” Biomarker testing, added Flora, allows targeting of cancer’s “Achilles heels.”
Barriers to this screening tool mostly impact the “least advantaged people,” he said.
The National Cancer Institute said last year, for example, that Black Americans have higher death rates from many types of cancers than white people.
Additionally, Black women are more likely to die from breast cancer than white women. And colorectal, lung and cervical cancers are more prevalent in Appalachian regions than in urban areas.