Study says allergy to red meat is under-diagnosed, probably due to clinicians’ limited knowledge of it, and Ky. is a national hotspot
Kentucky Health News
Thousands of Kentuckians are likely living with an allergy to red meat, and many of them probably don’t know it because it hasn’t been diagnosed in them, a new study suggests. Another study says most of the people who do the diagnoses — health-care providers — have little or no working knowledge of alpha-gal syndrome.
The studies were published Thursday by the Centers for Disease Control and Prevention. In the first one, scientists reviewed laboratory results of people who had been tested for antibodies that identify the syndrome since 2020. They found 110,000 suspected cases, but that figure is probably a significant underestimate,” reports Emily Anthes of The New York Times.
The second study, also done by CDC disease ecologist and veterinarian Dr. Johanna Salzer, “found that 78 percent of health-care providers who were surveyed had little or no knowledge of the condition, and many clinicians who had heard of the syndrome were not sure how to diagnose it,” Anthes reports. “When the researchers factored in this knowledge gap, they estimated that the true toll of the syndrome might be closer to a half-million, although Dr. Salzer acknowledged that the figure was ‘a crude estimate’.”
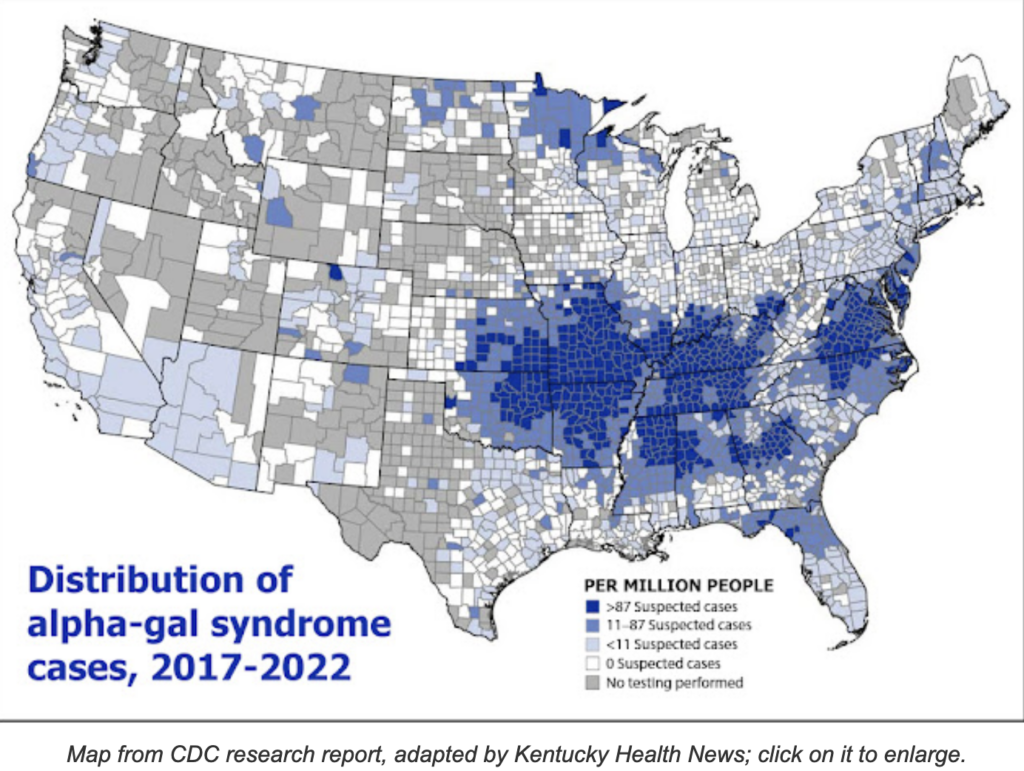
Extrapolating the national estimate of 450,000, about 6,000 Kentuckians would have the syndrome if they reflected the estimated national prevalence, but a map with the study shows that Kentucky is one of the states with the highest prevalence of the allergy, based on the available antibody tests.
Anna Buckman of the Adair County Community Voice reported in 2019, “Dr. Kourtney Gentry Gardner, an allergist-immunologist in Bowling Green, diagnoses about five people a month with the alpha-gal allergy, and it’s becoming increasingly more common, she says.”
Buckman noted that the syndrome “is relatively new to the allergy world,” having been identified in scientific literature about 15 years ago. Anthes reports, “Until August 2021, a single commercial lab did nearly all of this antibody testing in the United States. In one of the new studies, researchers reviewed the results of the antibody tests performed at this lab from 2017 to 2022.”
 The allergy “takes its name from galactose-alpha-1,3-galactose, a sugar present in beef, pork, lamb and the meat of most other mammals. (It is not present in humans or other apes.) Lone star ticks, which scientists believe are the primary culprits of the disease in the United States, can transmit the sugar to people through a bite. Some people’s immune systems may then label this foreign sugar a threat and overreact to its presence the next time they eat meat,” Anthes writes.
The allergy “takes its name from galactose-alpha-1,3-galactose, a sugar present in beef, pork, lamb and the meat of most other mammals. (It is not present in humans or other apes.) Lone star ticks, which scientists believe are the primary culprits of the disease in the United States, can transmit the sugar to people through a bite. Some people’s immune systems may then label this foreign sugar a threat and overreact to its presence the next time they eat meat,” Anthes writes.
The more a person is bitten, the more at risk they are of developing the allergy, Buckman reported.
“The symptoms, which often take hours to appear, are wide-ranging, and may include hives, nausea, diarrhea or anaphylactic shock,” Anthes reports. “Even patients who have the syndrome may not feel sick every time they eat meat.”