Attorney general files lawsuit against pharmacy benefit managers, manufacturers over alleged insulin pricing scheme
By Melissa Patrick
Kentucky Health News
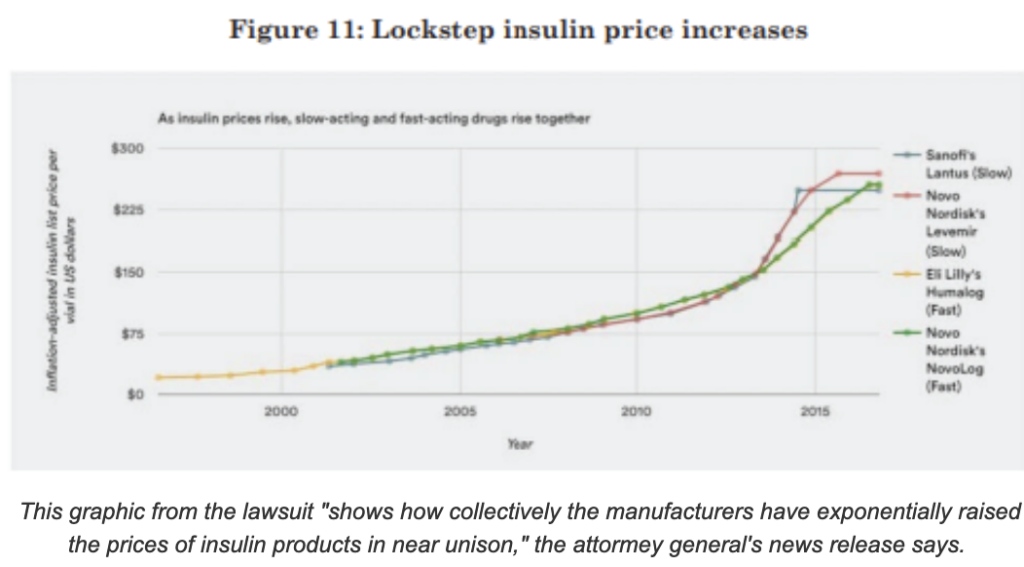
The lawsuit alleges that PBMs CVS Caremark, Optum Rx, and Express Scripts along with manufacturers Eli Lilly, Novo Nordisk and Sanofi have worked together to manipulate and increase insulin prices.
PBMs act as middlemen between insurance plans and drug manufacturers; they determine what drugs are offered, how much someone pays for the drug, and how much the pharmacists are paid.
A Cameron news release said, “The lawsuit alleges that instead of using such leverage to negotiate lower prices for their customers, PBMs have sought to increase their own profits by raising insulin prices. In that scheme, the insulin manufacturers artificially and willingly raised their reported prices and then deceptively refunded a significant portion of that price to PBMs through rebates, discounts, credits, and administration fees. . . . Executives for PBMs recently testified that between 75 and 84 cents of every dollar spent on insulin goes directly to affiliates of PBMs.”
Nearly 450,000 Kentuckians live with diabetes, and an additional 1.1 million are prediabetic.
Kentucky #insulin4all Chapter Advocate Angela Lautner told WKYT that it’s time for both manufacturers and PBMs “to be held accountable for the massive insulin prices we see here in the United States” and questioned why they exist at all.
“These lawsuits have been going on for a number of years, and it’s time that they come to a conclusion,” Lautner told the Lexington TV station. “Everybody knows that we are being taken advantage of and lives are literally being lost because of greed.”
Attorneys general from Arkansas, California, Illinois, Kansas, Louisiana, Mississippi, Montana, and Ohio have filed similar lawsuits in their states.
Kentucky lawmakers have been working on PBM issues for years, most recently passing 2020 Senate Bill 50 that among other things, required the state to hire a single PBM to manage Kentucky Medicaid’s prescription-drug business of more than $1 billion a year. Kentucky has saved at least $38 million from this move, money Gov. Andy Beshear has used to expand Medicaid benefits over objections of the Republican-controlled legislature. He and Cameron are running for governor.