Kentucky gets approval to expand and improve treatment for substance-use disorder among people on Medicaid
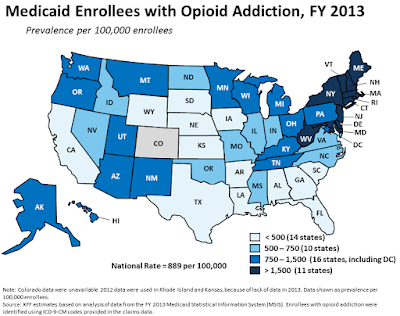
Kaiser Family Foundation map shows ranges of opioid addiction among
Medicaid beneficiaries before the program was expanded in 2014.
—
Kentucky has gained more flexibility to provide substance-use-disorder (SUD) services for people on Medicaid as part of the state’s new Medicaid plan, most of which was vacated by a judge in June, according to a state news release.
The Centers for Medicare and Medicaid Servicesapproved the “substance use disorder implementation protocol” portion of the plan, called Kentucky HEALTH, for “Helping to Engage and Achieve Long Term Health,” on Oct. 5. So far, it is the only part of the state’s request for a waiver of the rules to overhaul its Medicaid program that has been approved.
“Expanding access to treatment and recovery services for individuals with substance use disorder is critical to our efforts to combat the opioid epidemic in Kentucky,” Health Secretary Adam Meier said in a news release. “We have worked diligently to identify areas within the Medicaid program where care and treatment options can be expanded and improved. This demonstration waiver gives us the opportunity to help more Kentuckians get treatment and start on the path to recovery.”
The approval of this new program will expand access to SUD providers, will allow Medicaid to reimburse for short-term residential stays up to 30 days in mental-health facilities, and will allow Medicaid to pay for methadone, a drug used in medication-assisted treatment for addiction. It will also increase bed capacity for residential treatment facilities and will elevate program standards regarding the types of services, hours of clinical care and staff credentials.
In 2017, 1,565 people died in Kentucky from a drug overdose, up 11.5 percent from the prior year.
Kentucky Voices for Health, a consumer advocacy group, said this about the approval of expanded and improved SUD services in an email to members: “Kentucky Voices for Health and our partners applaud any efforts to combat the substance use disorder epidemic gripping our commonwealth. CMS approval of these services demonstrates that we can leverage our Medicaid program to be innovative and responsive to the needs of our Commonwealth without the harmful barriers the rest of the 1115 waiver would place in the way of Kentuckians struggling with addiction and other basic needs.”