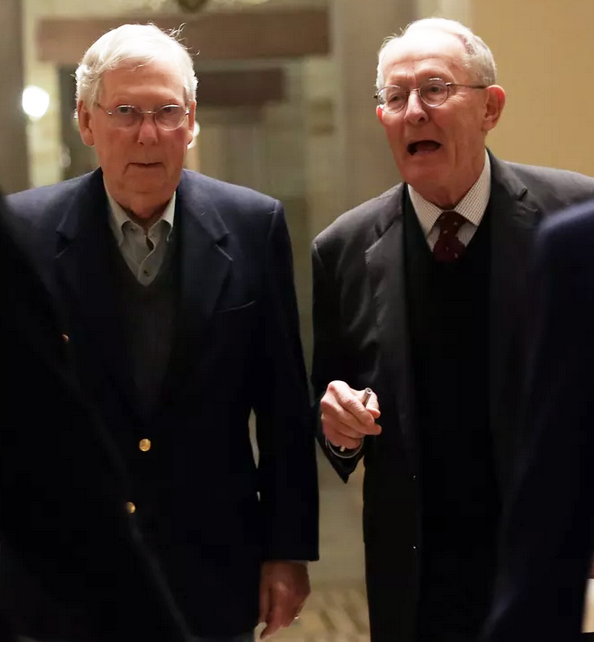
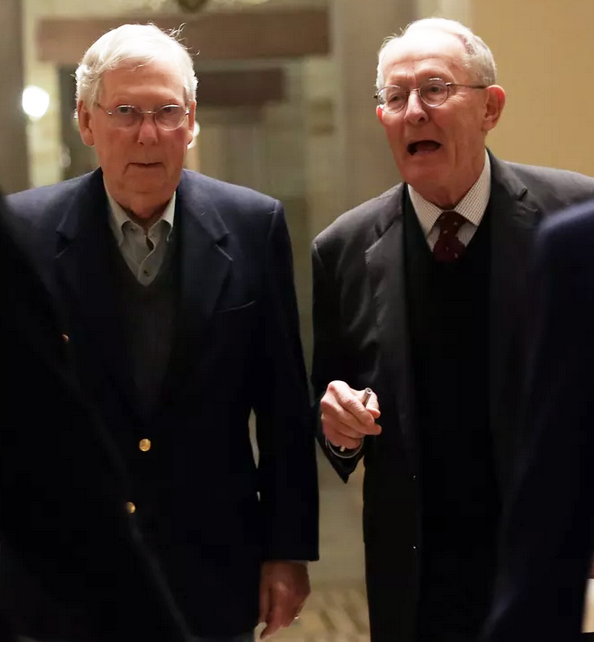
Negotiators reach compromise on surprise medical billing, but fate of the legislation may rest with Senate Majority Leader McConnell
Health insurance companies “are furiously lobbying Congress to tweak a last-minute deal on protecting Americans from surprise medical bills — one that is viewed as favoring doctors over them,” The Washington Post reports. “But they’re up against a ticking clock, heavy influence from private-equity-backed physician groups — and the reality that the pandemic boosted their profits even as medical providers suffered.”
The deal could be included in the must-pass measure to keep the government open, which could also include a massive pandemic relief bill. The fate of all could be in the hands of Senate Majority Leader Mitch McConnell, who “hasn’t said anything about it,” the Post reports. “His office didn’t respond to a query yesterday.”
Surprise billing is a problem in Kentucky. “A 2018 survey found that 32% of privately insured Kentucky adults reported receiving a medical bill that included an unexpected expense in the previous year,” Butler County Republican Party Chair Matthew Embry
wrote in a Dec. 2 piece for the
Courier Journal. “To make matters worse, 70% of patients who were hit with surprise medical bills had no idea they were receiving treatment from a provider outside of their insurance network. . . . If the patient can’t afford to pay astronomical surprise bills, they can be harassed by collection agencies, threatened with legal action and even forced into bankruptcy.”
McConnell “has not shown any particular interest in addressing surprise medical bills more generally, despite the national outcry over them,” Jordan Weissman
writes for liberal-leading
Slate. “The man tends to take his cues from the insurance industry (
Humana is based in Kentucky), which probably isn’t happy” about the latest plan. However, “The driving force for this deal in the Senate has been Tennessee’s Lamar Alexander, who is retiring this year, and who is extremely close with McConnell; the majority leader literally choked up while giving a goodbye speech to his friend from the
chamber floor. People genuinely think there’s a chance McConnell might let this pass as a last hurrah for his buddy.”
Embry concluded, “It is critical that Sen. McConnell focus his attention on passing fair, reasonable legislation to protect patients from surprise medical bills in the coming weeks. The financial future of hundreds of thousands of Kentucky residents depends on it.”
Dylan Scott of
Vox explains the issue: “One side of the debate (roughly represented by the first three committees to reach a deal, and the health-insurance lobby) wanted to default to something close to the average in-network price that is paid for the billed services in the area. The other side (represented by . . . the hospitals) wanted to use a third-party arbitration process to come up with a fair payment. The final deal, helpfully laid out by
the Brookings Institution’s Loren Adler on Twitter, is a compromise between the two. Read Loren’s thread if you want to get into all the wonky bits, but in brief:
- Surprise billing would be barred for out-of-network emergency care, for most out-of-network care at in-network facilities, and for air ambulances. The patients would be asked to pay only their in-network obligations for the care they received, and that is the end of it for them. The question then becomes what the insurer will pay the provider.
- There would initially be a 30-day period during which the insurance plan and the health care providers could try to negotiate a payment for the out-of-network claims. If they don’t reach an agreement, then arbitration would be the next step.
- The independent arbiters would primarily consider the average in-network charge for the services in question, as well as other information provider by the insurer and provider. Both sides would make an offer, and the arbiter would pick one based on the guidance stipulated in the bill.
“Nobody would call it a perfect plan — ground ambulances are notably excluded from the prohibition on surprise billing — but most health-policy experts seem to see it as a marked improvement over the status quo,” Scott writes, concluding that the bill’s touted $18 billion in savings could help make it part of a spending package that would add hundreds of billions to the national debt.
In another close look at the issue, the Post’s Paige Winfield Cunningham
writes, “Ensuring Americans don’t have to pay for out-of-network medical bills incurred through no fault of their own was expected to be a top priority for 2020. . . .The pandemic overtook most priorities on Capitol Hill, reshaping the legislative to-do list.”