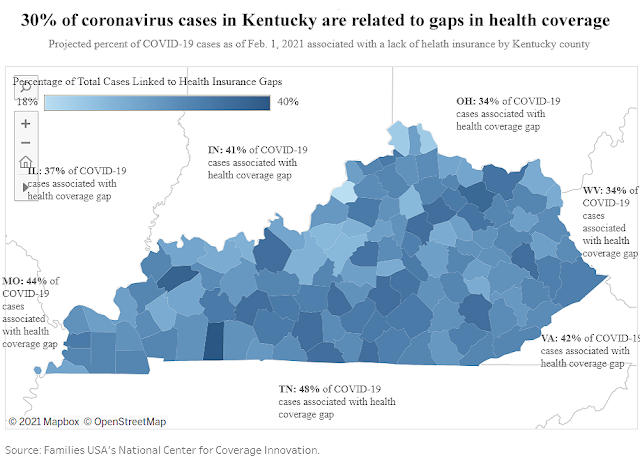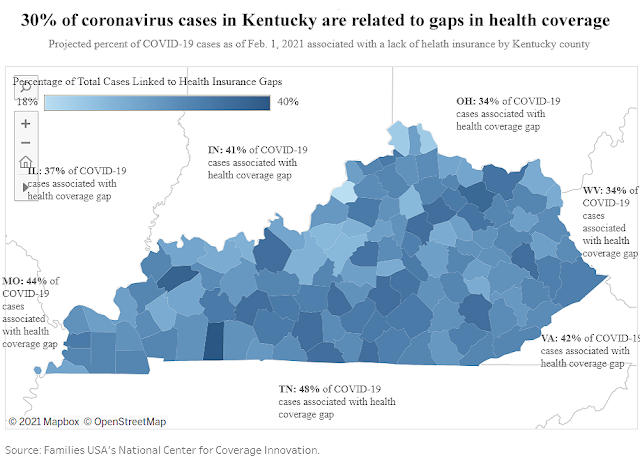
Chart by Dustin Pugel, Kentucky Center for Economic Policy; click on it to enlarge.
—–
By Melissa Patrick
Kentucky Health News
People living in communities with high rates of uninsured people were much more likely to get the coronavirus and to die from it than people living in communities with fewer uninsured people.
That’s according to a new Families USA report, “The Catastrophic Cost of Uninsurance: Covid-19 Cases and Deaths Closely Tied to America’s Health Coverage Gaps,” which found from the start of the pandemic through the end of August, every 10 percent increase in the proportion of a county’s residents who lacked health insurance was associated with a 70% increase in coronavirus cases and a 48% increase in Covid-19 deaths.
In that same period, the report found 30% of Kentucky’s total coronavirus cases (14,580 of 48,396) and 23% of the state’s Covid-19 deaths (217 of 933) were associated with gaps in health coverage.
“It seems clear to me that coverage matters when it comes to getting and staying healthy and Covid-19 is no exception,” said Dustin Pugel, policy analyst for the Kentucky Center for Economic Policy. “Kentucky moved really quickly, more so than our neighboring states, to make sure our folks were covered by a special Medicaid program when many lost their jobs and their health insurance with it. I can only imagine how much worse things might have been here if we had hundreds of thousands more without access to health care.”
Those changes helped give Kentucky the third highest percentage increase in Medicaid enrollment of any state between February and November 2020, according to state Medicaid Commissioner Lisa Lee.
Conversely, in the percentage of Covid-19 cases and deaths associated with health-insurance coverage gaps, Kentucky ranked low: 40th among the states, according to Families USA.
Its report provides numbers for counties with more than 50 cases or deaths. Todd County, at 40%, had the highest share of total cases linked to health-insurance gaps. Campbell and Boone counties, at 21% each, were lowest.
Fayette County, at 28%, had the highest percent of deaths linked to health-insurance gaps. Oldham County, at 14%, was lowest.
“Kentucky has had more people covered than our neighboring states and has fared much better in terms of both Covid cases and deaths,” said Emily Beauregard, executive director of Kentucky Voices for Health.
Thirty percent of Kentucky’s Covid-19 cases were linked to health coverage gaps, less than any adjoining state: 48% in Tennessee, 42% in Virginia and 34% in West Virginia, 34% in Ohio, 41% in Indiana, 37% in Illinois and 44% in Missouri. Kentucky’s Covid-related deaths that were linked to health coverage gaps were also lower than each of those states.
Every state saw some increase in Medicaid enrollment due to the pandemic started, but the percentage increase in Kentucky’s Medicaid rolls was more than any state but Oklahoma and Utah, Lee said.
The Beshear administration
launched a campaign to get more Black and Hispanic residents enrolled in health coverage as a way to reduce racial disparities in health.
 |
| Kaiser Family Foundation graph; click on it to enlarge. |
It also adopted a broad “presumptive eligibility” option, which is temporary, time-limited Medicaid coverage that allows the state to get people into the program quickly and before completing the full Medicaid application.
Data from Lee’s presentation at the May 20 Medicaid Oversight and Advisory Committee shows that in March 2020, the month the pandemic began, Kentucky had nearly 1.4 million people (1,383,005) in the program, with 2,573 signed up through presumptive eligibility.
Thirteen months later, in April 2020, that number had increased to nearly 1.7 million people (1,667,628), with 131,833 signed up through presumptive eligibility.
Of the newly enrolled, Lee said 52,797 of them are children and most are between the ages of 18-65, who qualified because of Medicaid expansion.
“This increase in enrollment reflects changes in our economy,” said Lee. ” Individuals have lost their jobs or they have reduced incomes.”
Lee added that Kentucky has qualified for a 6.2% increase in what the federal government reimburses for Medicaid since the pandemic hit and this has allowed the state to stay within its budget during the public health emergency.
Kentucky already had a low rate of uninsured residents —
6.4% in 2019 — mainly because the state expanded Medicaid to more low-income adults in 2013 under the Patient Protection and Affordable Care Act, which added about 450,000 people to the Medicaid rolls. Prior to the expansion, this program was limited to children, pregnant women, people with disabilities and people in nursing homes.
And as Kentuckians get back into the workforce, Lee and Beauregard both noted that Kentuckians who no longer qualify for Medicaid should look for coverage on the federal exchange since the Biden administration has extended a
special open enrollment period to Aug. 15. The special enrollment period includes enhanced premium subsidies, also known as tax credits, to help offset the cost of the health plans and also makes more people eligible for the subsides.
Lee said the state has been doing outreach to those who enrolled presumptively to help them complete that full Medicaid application that would move them over to the traditional Medicaid program. And if they no longer qualify for Medicaid, they work to help them gain coverage through the federal marketplace, commonly called Obamacare.
The Families USA report says it will use the findings from this report to ask one fundamental question, “If everyone in America had health insurance, how many people who contracted Covid-19 could have been spared, and how many who died might still be with us today?”
As of May 24, there have been at least 456,053 total cases of the coronavirus in Kentucky and 6,720 deaths, according to the
state’s daily report.