Rural Ky. needs more community health workers and medical-school residents, legislators and UK hospital executive say

By Al Cross
Kentucky Health News
Improving health care and health in rural Kentucky will take more people in the health-care workforce, specifically at the top and bottom of the pay scale, two key legislators and one of the state’s top hospital administrators said Tuesday, June 8.
Kentucky needs more health-care workers overall, because it may lose some to the pandemic, Mark Birdwhistell, vice president for health services administration at the University of Kentucky and chief of staff for UK HealthCare, said during a Kentucky Chamber of Commerce webinar on rural-urban health disparities.
“Coming out of Covid . . . many of our clinical workforce are fatigued, and they’re second-guessing: ‘Is this the career path that I want to go on?’ They’ve been in combat for a year and a half now,” Birdwhistell said.
State Rep. Kim Moser, a Republican from Taylor Mill in Northern Kentucky, agreed. “Burnout is real,” she said, noting that her husband is a pulmonologist who has treated Covid patients.
“Just because you’ve got coverage doesn’t mean you’ve got access” to the health care you need, Birdwhistell said, because “Many providers don’t take Medicaid.” He and Baptist Health Louisville President Larry Gray said health insurance tends to cost more in rural areas due to lack of competition, so people buy policies with high co-payments and deductibles.
The expansion of Medicaid made clearer how the “social determinants of health” leave rural areas with lower health status, Birdwhistell said. It’s twice as likely for someone in an urban area to finish high school or college as someone in a rural area, he said, so health literacy is lower in rural areas. And that extends to health insurance, he said, giving one example: “Deductible. That’s hard to explain in English.”
Moser, a retired nurse who chairs the state House Health and Family Services Committee, said expanding the limited government and commercial-insurance reimbursement for community health workers’ services would help. “That is one policy that we’re looking at possibly expanding,” she said.
Birdwhistell said that would be “very, very cost-effective,” because “In a lot of communities, people don’t know how to access care, and they show up in the emergency room. And that is probably the worst place for anybody to show up with a high fever, strep throat, whatever. They don’t get a continuum of care. . . . They will listen to somebody that they grew up with, somebody that they go to church with, somebody that they see on the soccer field with their kids.”
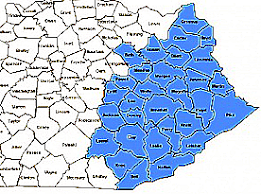
Eastern Kentucky already has the third largest concentration of community health workers in the nation, trailing only Alaska and northwest Mississippi, according to the Bureau of Labor Statistics.
Nationally, CHW pay averages $46,000 a year, but in Kentucky the average is $37,320.The webinar discussion also addressed the need for more doctors in rural Kentucky.
Birdwhistell said a major obstacle to getting more physicians in rural areas of the state are the limits on federally funded residency slots at the UK and University of Louisville medical schools. “Flipping that switch could pretty instantly change the number of professionals we have coming out,” he said.
Republican Sen. Ralph Alvarado of Winchester, a physician, agreed, saying that residents tend to set up practices within 80 miles of where they do their residency. Moser also endorsed the idea.
Gray said the shortage is especially bad in Eastern Kentucky, which needs providers who are willing to come to the region with “a sense of mission and vocation.” But even with enough providers, transportation to get some patients to them is still an obstacle in some areas, he said. The expansion of telehealth has helped, he said, but some areas still lack internet access that is fast enough for it.
And even with telehealth, a shortage of specialists blocks care. For example, Kentucky has only 59 child psychiatrists, and half of them “are cash-only, don’t take insurance,” Alvarado said.
The panel started out by discussing some of the state’s poor health statistics. Alvarado said the use of tobacco is heavier in rural areas, leading to all sorts of health issues, and obesity is more common, causing “more negative outcomes.”
The news isn’t all bad, he said, noting how Kentucky has raised its screening for colon cancer from 47th to 19th in the nation. “That’s going to rub off on our death rates . . . in 10 years,” he said. “There is some hope.” But he also noted that screening rates in Eastern Kentucky remain relatively low.