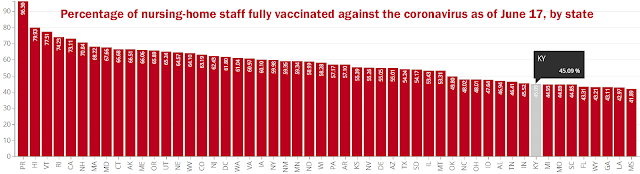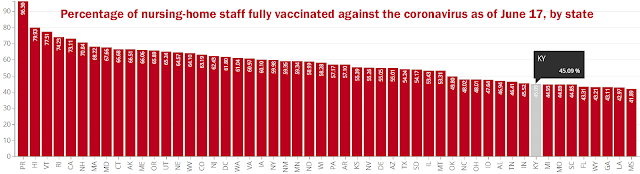
Centers for Medicare and Medicaid Services graph, adapted by Ky. Health News; click it to enlarge
—–
Employees providing care at Kentucky nursing homes are among the least likely in the country to be vaccinated against the coronavirus, which has killed almost 2,500 people in those nursing homes.
The extent of the problem could be worse, because only about a third of the state’s nursing homes have reported vaccination figures to the Centers for Medicare and Medicaid Services, which pays most of their costs and regulates them.
The latest update of
the database, June 17, showed that 45.09 percent of the health-care employees at reporting nursing homes had been fully vaccinated for the virus. That was ninth lowest among the states.
Sherry Culp, state government’s long-term-care ombudsman, told the Lexington Herald-Leader, “My concern is that having staff who are not vaccinated coming into these places every day and working in close proximity with residents could increase the incidence of Covid once again.”
Culp noted that 78% of nursing-home residents are fully vaccinated, and Herald-Leader reporter John Cheves notes that the homes had only 13 active cases in Wednesday. But he notes, “The state already
saw one tragedy this year,” at a nursing home in Morehead, “when an unvaccinated worker brought in the virus and infected 46 people. Three people died, including a vaccinated resident.”
A study of the outbreak found that it was caused by a mutated variant of the virus. Health experts warn that unvaccinated people are breeding grounds for more variants, which can be more contagious and/or more deadly. Current vaccines seem largely effective, but the Delta variant that is 6 to 10 percent of U.S. cases and is expected to become dominant requires two doses of
Pfizer vaccine to be suppressed. One dose is only 33% effective, research indicates.
Nursing homes say they don’t want to require shots, for fear of losing employees at a time when the workforce is tight. They also cite “skepticism about the safety and effectiveness of the vaccine, particularly for women of child-bearing age” and the belief that they are immune to the virus because they have been exposed to it, “an assumption that is
not always accurate,” Cheves writes.
Betsy Johnson, president of the Kentucky Association of Health Care Facilities, the state nursing-home trade group, told Cheves, “The most successful strategies that we have seen are personal discussions with mentors, colleagues and experts to dispel fears and mistruths. Businesses are choosing to use approaches that are friendly and less forceful to manage those who are reluctant of the government. We continue to push vaccine efforts and are hopeful to see an increase among our front-line workers.”
At Cumberland Valley Manor in Burkesville, where only 23% of health-care workers are fully vaccinated, Administrator Mary Beth Shelton told Cheves, “We’re giving them the facts, we’re giving them the statistics. I’ve personally had the vaccine and I’ve had no side effects, and I talk about that.”
Shelton said the reason she hears most from employees for not getting vaccinated “is that it’s new on the market and it’s not FDA-approved yet, so they have doubts about it.” The Food and Drug Administration has approved three vaccines for emergency use and is expected to give at least one full approval this fall.
Most nursing homes are owned by chains. “Culp says she has spoken to Kentucky nursing home administrators who are privately advising their facilities’ corporate owners to consider making vaccination mandatory for employees, Cheves reports, and a federal judge in Texas has ruled that they can.
But in rural places like Burkesville, requiring vaccination is not practical, Shelton told Cheves: “I would hate to lose anybody because of that. The reality of the situation is that it’s just not doable in our setting, especially in rural areas where we fight for staff. It’s just not possible for us.”
One thing nursing homes will feel compelled to do, starting June 20, is report their vaccination data. On that date, CMS says “Failure to meet these new reporting requirements will result in a [penalty] starting at $1,000 for facilities with no previous occurrences of noncompliance.”