Federal audits reveal widespread overcharges, other errors in Medicare Advantage plans; Humana and United stand out
By Fred Schulte and Holly K. Hacker
Kaiser Health News
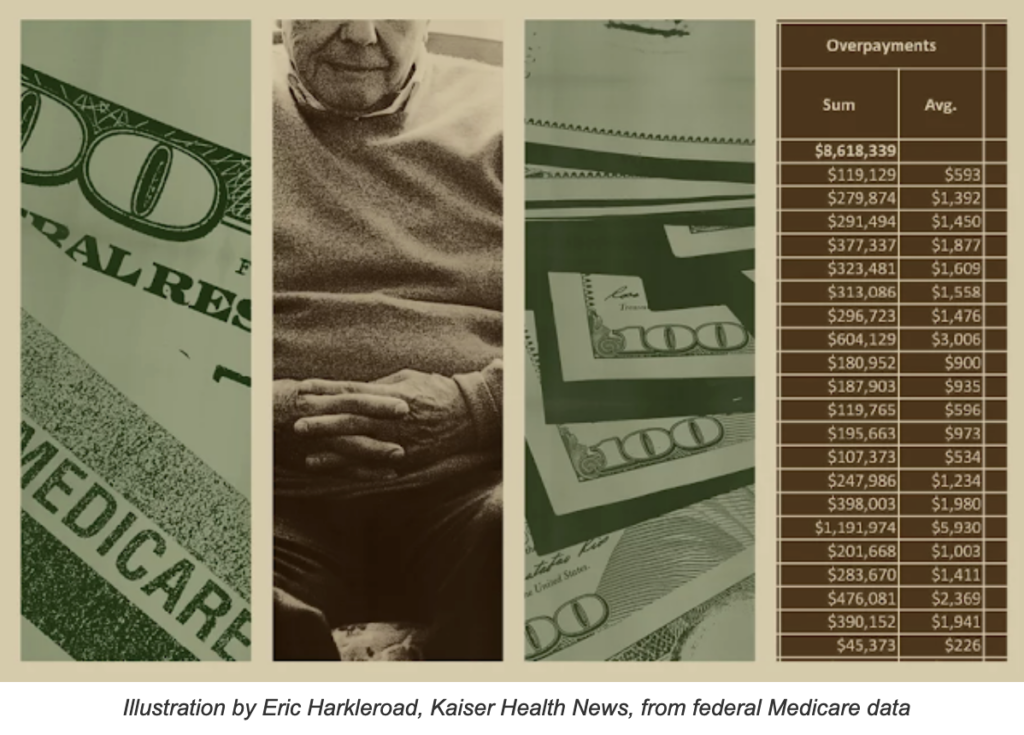
Recently released federal audits reveal widespread overcharges and other errors in payments to Medicare Advantage health plans, with some plans overbilling the government more than $1,000 per patient a year on average.
Summaries of the 90 audits, which examined billings from 2011 through 2013 and are the most recent reviews completed, were obtained exclusively by Kaiser Health News through a three-year Freedom of Information Act lawsuit, which was settled in late September.
UnitedHealthcare and Louisville-based Humana, the two biggest Advantage insurers, accounted for 26 of the 90 contract audits over the three years.
Eight audits of United plans found overpayments, while seven others found the government had underpaid. Humana’s 11 audits with overpayments included plans in Florida and Puerto Rico that CMS had audited twice in three years.
The Florida Humana plan also was the target of an unrelated audit in 2021 by the Department of Health and Human Services inspector general. That audit, which covered billings in 2015, concluded Humana improperly collected nearly $200 million by overstating how sick some patients in its Medicare Advantage plans were. Officials have yet to recoup any of that money, either.
In an email, Humana spokesperson Jahna Lindsay-Jones called the audit findings “preliminary” and noted they were based on a sampling of 2015 claims.
“While we continue to have substantive concerns with how CMS audits are conducted, Humana remains committed to working closely with regulators to improve the Medicare Advantage program in ways that increase seniors’ access to high-quality, lower cost care,” Lindsay-Jones wrote.
How Medicare Advantage works
When auditors came calling, the previously hidden CMS records show, they often found little or no support for diagnoses submitted by the Advantage plans, such as chronic obstructive pulmonary disease, diabetes, or vascular disease. Though auditors look at the records of a relatively small sample of patients, they can extrapolate the error rate to the broad population of patients in the Medicare Advantage health plan and calculate millions of dollars in overpayments.
Overall, CMS auditors flagged diagnostic billing codes — which show what patients were treated for — as invalid more than 8,600 times. The audits covered records for 18,090 patients over three years.
In many cases, auditors found that the medical credentials of the health-care provider who made the diagnosis were unclear, the records provided were unacceptable, or the record lacked a signature as required. Other files bore the wrong patient’s name or were missing altogether.
The rates of billing codes rejected by auditors varied widely across the 90 audits. Seven health plans had fewer than 10% of their codes flagged, but the rate of invalid codes topped 80% at a defunct New York HMO.
One Medicare Advantage health plan submitted 57 hardship requests, more than any other insurer, though CMS approved only six. In three cases, the health plans said the records were destroyed in floods. Another cited a warehouse fire, and two said the records couldn’t be turned over because a doctor had been convicted for his role in illegally distributing millions of oxycodone pills through his network of pain clinics.
Other Medicare Advantage health plans said they had no luck retrieving medical records from doctors who had moved, retired, or died — and in some cases been arrested or lost their licenses for misconduct.
CMS found most excuses wanting, telling health plans that it granted exceptions only in “truly extraordinary circumstances.” CMS said it receives about 100 of these requests for each year it audits and approves about 20% of them.
Dara Corrigan, a CMS deputy administrator, said that as a “general matter,” its Medicare Advantage audits “are not designed to detect fraud, nor are they intended to identify all improper diagnosis submissions.”
Protecting Taxpayers
The costs to taxpayers from improper payments have mushroomed over the past decade as more seniors pick Medicare Advantage plans. CMS has estimated the total overpayments to health plans in the 2011-13 audits at $650 million, but how much it will eventually claw back remains unclear.
Payment errors continue to be a drain on the program. CMS has estimated net overpayments to Medicare Advantage plans triggered by unconfirmed medical diagnoses in 2022 at $11.4 billion.
“This isn’t a partisan issue,” said Sen. Sherrod Brown (D-Ohio). “I’ve requested a plan from CMS as to how they plan to recoup these taxpayer-funded overpayments and prevent future overbilling.”
Leslie Gordon, acting director of health care for the Government Accountability Office, the auditing arm of Congress, said CMS needs to speed up the audit and appeals process to get quicker results.
“That is money that should be recovered,” Gordon told Kaiser Health News.
As Medicare Advantage faces mounting criticism from government watchdogs and in Congress, the industry has tried to rally seniors to its side while disputing audit findings and research that asserts the program costs taxpayers more than it should.
America’s Health Insurance Plans, an insurance industry lobby, criticized Kaiser’s reporting on the newly released audits as “misleading,” while the pro-industry group Better Medicare Alliance said the audits were “in some cases, more than a decade old.”
Jeff De Los Reyes, a senior vice president at the GHG Advisors health-care consulting group, said he believes the health plans have improved their documentation in recent years. But, he said, “Coding is never 100% perfect and there will be errors despite the best of intentions.”
Rep. Katie Porter, a Democrat from Southern California and a critic of Medicare Advantage, countered: “When big insurance bills taxpayers for care it never intends to deliver, it is stealing our tax dollars.”
Kaiser Health News is a national newsroom that produces in-depth journalism about health issues. Together with policy pnalysis and polling, KHN is one of the three major operating programs of the Kaiser Family Foundation, an endowed nonprofit organization providing information on health issues to the nation.