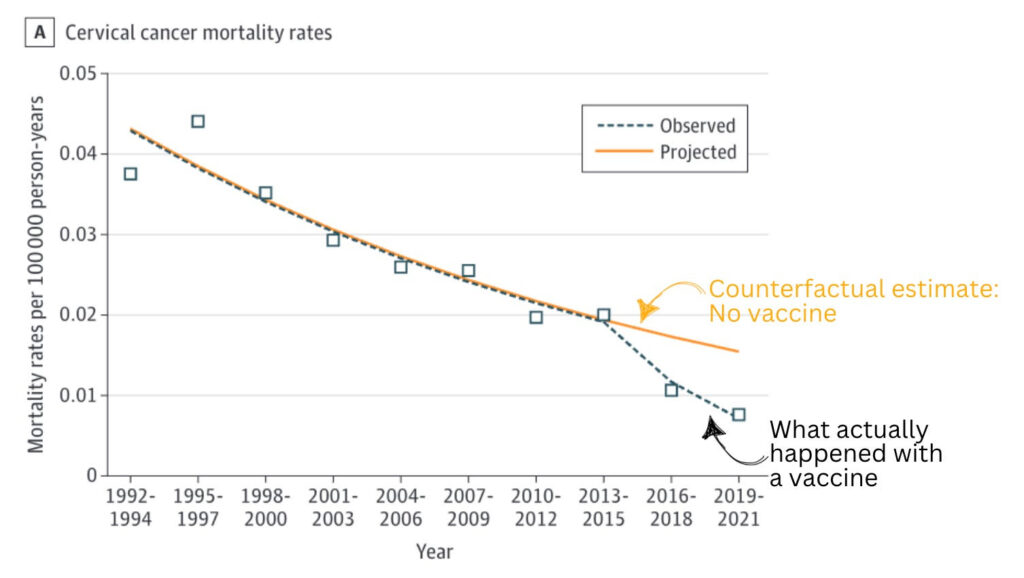
“Assuming that the trend from 1992-1994 to 2013-2015 would have continued, an estimated 26 additional cervical cancer deaths would have been expected to occur between 2016 to 2021, based on projected mortality rates,” the authors wrote.
Study: Cervical cancer deaths drop in women under 25, and researchers credit HPV vaccine; Ky. ranks 44th for HPV vaccine
By Melissa Patrick
Kentucky Health News
A study, published in JAMA Network, shows the effectiveness of human papillomavirus (HPV) vaccines in reducing deaths from cervical cancer in women under 25.
Among women under the age of 25, the first group vaccinated, the study found a 62% drop in deaths from cervical cancer in the United States. The HPV vaccine has been recommended to young women since 2006.
“This is a huge public-health success story,” Ashish Deshmukh, co-leader of the cancer prevention and control research program at the Medical University of South Carolina’s Hollings Cancer Center, and senior author of the research, told the Washington Post. “Vaccination is the only explanation for this startling and substantial decline.”
The researchers used data from the National Center for Health Statistics and looked at cervical cancer deaths in three-year blocks of time.
Between 1992 and 2021, there were 398 cervical cancer deaths reported among women younger than 25. From 1992-1994 to 2013-2015, mortality from cervical cancer gradually declined 3.7 % each year and from 2013-2015 to 2019-2021, it decreased 15.2% per year, according to the study. The number of deaths decreased from 55 in 1992-1994 to 35 in 2013-2015 to 13 in 2019-2021.
Deshmukh told the Post that he expects to see cancer deaths continue to fall as this group ages because there is a higher burden of cervical cancer in women in their 30s and 40s.
About the study, Katelyn Jetelia, the founder of Your Local Epidemiologist, writes, “It looks like the vaccine supercharged the decline” and that “the causal argument is very strong.” She said that’s because “there’s a consistent and strong effect across different populations; there’s biological plausibility (HPV causes cervical cancer, and there was an intervention that we know works on a biologic level), and; this was the first cohort of women widely advised to get vaccinated.”
“The findings from this study highlight the urgency to improve HPV vaccination coverage,” the researchers said in a letter.
HPV Vaccines and Kentucky
This is especially true in Kentucky, which has low HPV vaccination rates and leads the nation in the rate of cases of and deaths from cervical cancer.
In 2022, Kentucky ranked 44th in HPV vaccination, with only 55% of teens 13-17 having received all recommended doses, according to America’s Health Rankings. That was a decline from the 57% reported in 2021 and well below the national average of 63%.
The vaccine’s greatest obstacle appears to be that it is associated with a sexually transmitted disease. Researchers have said improving the vaccination rate depends on changing the perception that the vaccine is something that prevents STDs to the knowledge that it primarily prevents cancer.
The HPV vaccine protects against six cancers: cervical, anal, penile, vaginal, vulvar and head or neck. According to the Centers for Disease Control and Prevention, it can prevent over 90% of sexually transmitted cancers caused by HPV from ever developing.
Two doses of the HPV vaccine are recommended for all 11- and 12-year-olds, but the series can begin at 9. It is also recommended for those 13 to 26 if unvaccinated; three doses are recommended for people who get their first dose at 15 or later, and for people with certain conditions that weaken immunity.
In addition, it is also recommended that anyone between 27 and 45 who is not vaccinated should talk to their health-care provider about their risk of infection and the benefits of getting vaccinated.