Federal panel says PSA screening for prostate cancer does more harm than good, but no better test is available
 |
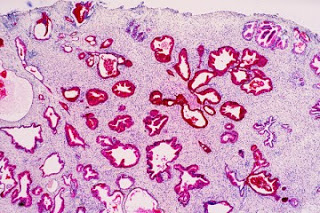
| Prostate cancer cells. Getty Images photo by Abbey Michael. |
An influential federal panel says testing healthy men’s prostate-specific antigen levels to detect prostate cancer does more harm than good.
The PSA test can lead to unnecessary biopsies for men who turn out to be cancer-free. Those biopsies can also lead to men being treated for cancers that are so slow-growing (a characteristic of most prostate cancers) that they didn’t need to be detected.
An estimated 1,000 to 1,300 men die annually from complications associated with treatments that are initiated because of PSA screening, reports Alice Park for Time magazine. Moreover, treating harmless prostate tumors increases the chances of making men impotent or incontinent.
The U.S. Preventive Services Task Force published the recommendation in the Annals of Internal Medicine. In 2009, the panel also recommended that women delay routine mammograms until the age of 50. That was controversial, and “The task force’s recommendation goes against two decades of widespread use of the PSA test, a $35 blood test,” Park reports.
“The recommendation is not just counter to what the lay public has been taught about cancer prevention but what physicians have been taught as well,” said Dr. Michael LeFevre, co-vice chair of the USPSTF and a professor of family and community medicine at University of Missouri. “We’ve been told for decades to be afraid of cancer and that the only hope is early detection and treatment. So it’s hard for physicians and patients alike to accept that not all cancers need to be detected or need to be treated and that there are harms associated with screening, not just benefits.”
Through PSA testing, physicians “were finding the cancer earlier, so the time from diagnosis to death was longer, but the patient wasn’t actually living longer,” explained Dr. Otis Brawley, chief medical officer of the American Cancer Society.
But there isn’t a better test to replace the PSA, and Ian Thompson, chairman of urology at the University of Texas Health Science Center, said to reject it completely is unwise. He said U.S. death rates from prostate cancer dropped between 30 and 50 percent since the screening became commonplace in the early 1990s, though those numbers could also have been influenced by more effective treatments. Thompson said he didn’t want to go back to the “bad old days” when doctors only found prostate cancer when it was already unable to be cured, reports Liz Szabo for USA Today. (Read more)