Study finds Kentuckians on Medicaid expansion make heavy use of preventive screenings
“One of the benefits of getting more people insured is that they take advantage of the preventive services that can lead to improved health and lower health care costs in the long run,” Ben Chandler, president and CEO of the foundation, said in a news release. “That positive trend is what we’re seeing in Kentucky in terms of breast and colorectal cancer screenings, preventive dental services and diabetes and hepatitis C screenings for Kentuckians with low incomes.”
These findings come as no surprise, since those who qualify for Medicaid under the expansion (to those who earn up to 138 percent of the federal poverty line) often work at low-paying jobs that don’t provide health insurance, are students or are caretakers and have gone without health insurance for a long time.
Since the implementation of the Patient Protection and Affordable Care Act and the state’s expansion of Medicaid, Kentucky’s uninsured rate has dropped by more than half, from 14.3 percent in 2013 to 6 percent in 2015 respectively, according to the report.
One of the 10 essential benefits of the reform law is free preventive health care, a benefit that thousands of Kentuckians have taken advantage of.
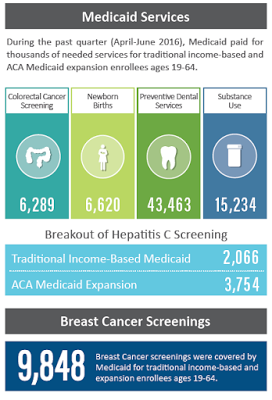
The study found that in the second quarter of 2016, Medicaid paid for 9,848 breast cancer screenings, with 87 percent of them (8,500) for Kentuckians covered by the expansion. The other 1,251 screenings were for patients who qualified under traditional Medicaid.
This was similar to the same time frame last year, when 88 percent of the 10,191 breast screenings were for those covered by the expansion.
“Screenings for breast cancer among those living on lower incomes can be particularly important because, statistically, low-income women have a higher risk of not being diagnosed until the later stages of breast cancer,” Chandler said. “If doctors can catch the cancer early with regular mammograms so patients can get treatment at the earlier stages, we’re talking about saving lives while also reducing long-term costs.”
 |
| Foundation for a Healthy Kentucky graphic on Medicaid preventive services in Kentucky |
This trend of increased screenings by the expansion population also held true for other screenings during the second quarter: 88 percent of the 6,289 colorectal cancer screenings; 79 percent of the 4,589 diabetes screenings; and 65 percent of the 5,820 hepatitis C screenings.
The report also found that Medicaid covered 43,463 preventive dental screenings between April and June and that 76 percent, or 32,968, were for expansion patients.
“In my experience, Medicaid expansion patients first used their plans at the dentist to address dental neglect in hopes of eliminating pain and getting prepared for the workforce. It is very difficult to concentrate in school or at work with a toothache,” Laura Hancock Jones, chair of the Kentucky Oral Health Coalition and a member of the foundation’s Community Advisory Committee, said in the release.
Medicaid has also seen a big jump in substance-abuse treatment, from 5,675 services during the first quarter of 2015 to 15,234 during the second quarter of 2016, says the report. More than 56,600 substance-abuse treatment services have been covered by Medicaid in those 18 months.
Mental-health benefits and the treatment of substance-abuse disorders are also benefits required under federal health reform.
“Substance abuse is one of the most critical health and safety issues facing Kentuckians,” Chandler said. “Overdose deaths continue to climb, and addiction exacts a terrible emotional, financial and physical toll on families.”
Medicaid also covered 6,620 births, 1,769 of which were delivered by expansion patients, during the second quarter of this year.
The report comes from the State Health Access Data Assistance Center at the University of Minnesota, which the foundation is paying more than $280,000 to study the impact of the Patient Protection and Affordable Care Act over three years.
Kentucky’s health rankings are poor in just about every category, with some of the highest rates of cancer, diabetes, obesity, stroke and heart disease in the nation. Health advocates look for improvements in these rankings to come from long-term preventive care, which many now have because of health reform and the expansion.
But health advocates and many Kentuckians on Medicaid are concerned about what will happen to these benefits if the state’s Medicaid program is changed, as Gov. Matt Bevin has proposed, or health reform is repealed, as President-elect Donald Trump has promised.
Bevin says the state can’t afford to have nearly one-third of its population on Medicaid and has submitted a proposal to the federal government to let the state require beneficiaries to pay monthly premiums and require non-disabled recipients to work or to do community service. It also requires some of the currently covered benefits, like vision and dental, to be earned through a rewards program. The plan is currently under negotiation with federal officials.
The expanded population is paid in full by the federal government through the end of this year. In 2017, the state will be responsible for 5 percent of the cost, rising in annual steps to the reform law’s limit of 10 percent in 2020. Bevin’s proposal says this plan “is expected to save taxpayers $2.2 billion over the five-year waiver period,” by reducing enrollment in the program, but only $331 million of that would be state tax money, because the federal government covers the bulk of Medicaid costs.
President-elect Donald Trump and the GOP-controlled Congress have promised to repeal health reform, though Trump has said insurance companies should still have to cover pre-existing conditions. Republicans in Congress have long wanted to turn Medicaid into a block-grant program, largely run by the states.
