Kynect tries to get more eligible people to sign up for subsidized insurance, disputes report that 2/3 of eligible haven’t enrolled
Kentucky Health News
State officials recognize that there is a shortfall in the number of people who have signed up for subsidized health-insurance plans through Kynect, the state insurance exchange, but disputes the recent report that two-thirds of eligible people have yet to take advantage of the opportunity.
“We do not feel the numbers related to the two-thirds are correct,” Gwenda Bond, a spokeswoman for the Cabinet for Health and Family Services, said in an email. “The figures cited to arrive at that conclusion were preliminary estimates for Medicaid expansion and qualified-health-plan subsidy eligibility based on Census data, completed prior to the first open enrollment period.”
Qualified health plans are bought through Kynect, with the premiums reduced by a federal subsidy, structured as a premium tax credit.
She noted that Kentucky more than doubled the number it expected to enroll in Medicaid through the ACA and “some people who were originally assumed to qualify for subsidies qualified for Medicaid instead.”
Why does it matter?
Insurance markets depend on a mix of healthy people paying premiums to subsidize the medical cost of others. In Kentucky, those who enrolled in both private insurance and Medicaid through Kynect have had more health issues, which has caused insurance companies to pay more claims than expected and raise rates.
WellCare is the only insurance company on Kynect that will lower its premiums next year, by an average of 11 percent. CareSource is increasing them by an average of 11.8 percent, Anthem by 12.2 percent (0.4 percent for small groups); Humana by 5.2 percent (7.8 percent for small groups); and Kentucky Health Cooperative, which sold three-fourths of private policies on Kynect and lost $50 million, by 25 percent.
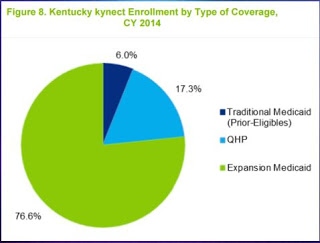
Kentucky has 1,264,275 people on Medicaid, with almost 400,000 of them signed up through the expansion, which includes those who make up to 138 percent of the federal poverty level. About 100,000 Kentuckians bought a qualified health plan.
Initially, the U.S. Department of Health and Human Services said about 40 percent of the policies sold on exchanges should cover people between 18 and 35, the most healthy group, to keep the exchanges financially stable. Recent HHS data states that this group accounted for only 28 percent of the policies nationally in 2014 and 2015.
Efforts to get qualified people to buy insurance
Kynect works to reach both the uninsured who are not eligible for Medicaid but are eligible for subsidies, as well as those who have bought or are planning to buy insurance in the individual market but are unaware that they may qualify for subsidies through Kynect.
“We have always anticipated that educating consumers and enrolling individuals who were eligible for subsidies would be a years-long process, as this facet of the Affordable Care Act is entirely new,” Bond said.
One of the exchange’s most recent efforts is a media campaign. It encourages those who have bought insurance in the individual private market, and who plan to renew their policies before open enrollment begins Oct. 19, to check rates on Kynect first — and informing them that they can enroll now if their coverage period is ending. Open enrollment runs through Dec. 11.
Kynect is also emphasizing that some areas of the state will have up to eight insurers to choose from this year, Bond said.
The exchange added some new events for outreach this year, including a “Kynect All Access Lounge” at the Forecastle Music Festival in Louisville this summer and extending the hours that “Kynectors,” employees who help people navigate the system, are available at local Cooperative Extension Service offices.
